Wellcome Global Monitor 2020: Covid-19
Read more about why people worldwide are not sure their governments value science.
Covid-19 isn’t the first time the world has had to deal with a global pandemic – and it won’t be the last. But lessons learned from previous disease outbreaks, such as HIV/AIDS, play a key role in providing the tools and insight to prepare for, control and eventually prevent future pandemics.
Tom Levy/San Francisco Chronicle via Getty Images
When reports of a deadly new disease reached the public in January 2020, it was met first with indifference, then confusion and then fear. Eventually, as the mystery SARS-CoV-2 virus spread across the world, governments, scientists and world leaders scrambled to react.
For anyone who could remember the first outbreaks of HIV in the 1980s, this was hauntingly familiar.
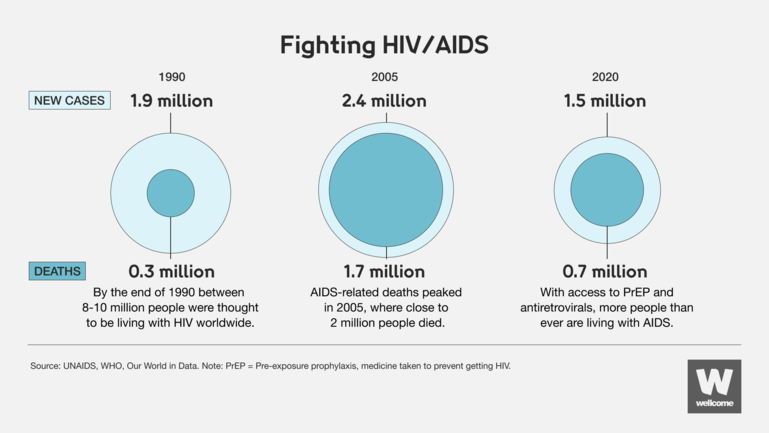
Over 40 years since the first recorded case, HIV/AIDS is still a major global public health issue. In 2020 an estimated 37.7 million people were living with HIV and 680,000 people died of AIDS-related illnesses.
Wellcome
The comparison offers a sombre reminder of the devastating toll of pandemics, and how failure to prepare or work together in a global response can have enormous consequences.
The HIV/AIDS community has had its share of life-saving victories, as well as losses. Important lessons should be learnt from both to guide our way out of this pandemic and prevent the next.
Early cases of HIV led scientists and healthcare workers to think that the virus was only a risk to drug users and members of the LGBTQ+ community. While it was quickly proven to be a risk to everyone, unclear communication and a crumbling trust in governments allowed this harmful narrative to shape public opinion and public health responses for decades.
Without accurate information about how the virus spread and who it could infect, HIV was able to transmit through populations with relative ease. At the same time, a lack of trust in government and healthcare providers made those living with HIV less likely to access proper treatment.
This shows the dangers of mistrust and misinformation in public health, and we are seeing a similar problem during the Covid-19 pandemic.
Early denial, lack of transparency and conflicting messaging from governments and scientists have again caused confusion and mistrust around the world, with a relentless stream of online misinformation and conspiracy theories adding fuel to the fire.
During the first phase of the Covid-19 pandemic, the Wellcome Global Monitor 2020 report found a clear link between people’s trust in government and their belief that their government trusts science. Yet globally, only a quarter of those surveyed said that their government values the opinions and expertise of scientists ‘a lot’.

Read more about why people worldwide are not sure their governments value science.
If governments want to build back public trust, they need to prioritise transparent leadership, clear communication and public health decisions informed by science. For those that do, the benefits are clear. In countries like Denmark, high trust levels have already led to increased rates of vaccine uptake and lower Covid-19 infection rates, contributing to one of the lowest Covid-19 death rates in Europe.
A programme for a global response to HIV/AIDS was only developed six years into the pandemic. By that time, the virus had already exposed and exacerbated huge inequalities in social, economic and healthcare systems around the world.
Though we have come a long way over the past 40 years, many of the most affected communities still need better access to treatments and testing. The majority of people now living with HIV are in low- and middle-income countries, with East and Southern Africa regions accounting for more than two-thirds of cases worldwide.
Wellcome
We cannot allow history to repeat itself with Covid-19.
To end this pandemic the international community must come together to make sure everyone has access to vaccines and treatments, as well as the tools to track the virus to prevent future outbreaks.
Programmes such as the Coalition for Epidemic Preparedness Innovations (CEPI) and COVAX will be crucial to ending the Covid-19 pandemic and preventing the next.

Wellcome and the Bill & Melinda Gates Foundation have both pledged $150 million each to the Coalition for Epidemic Preparedness Innovations.
A pandemic, by its definition, affects a large number of people across multiple demographics, communities and geographies. Depending on who and where you are, you are likely to experience the impacts of the disease in different ways.
Therefore, interventions that work for one group of people may not work for another.
It didn’t take long for health officials to learn that “don’t share needles” was not an effective message for limiting the spread of HIV amongst drug users in the USA. Similarly, the guidance “Abstain, Be Faithful and Use Condoms” – a public health initiative that was successful in decreasing HIV infection rates in Uganda – has been less effective in other parts of Africa where gender inequality and a lack of access to contraception or sex education remain an issue.
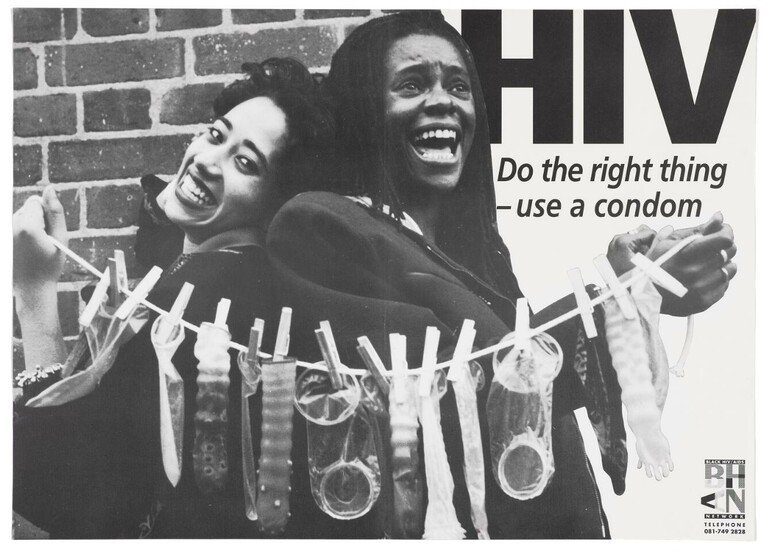
Black HIV/AIDS Network via Wellcome Collection
This is a familiar challenge for the Covid-19 response. Washing your hands and working from home is unhelpful advice to a community where running water, soap and home-working are not easily accessible. While a nationwide lockdown is especially problematic if the government can’t provide communities with income support, health services and access to food and water.
As we see the burden of the Covid-19 pandemic move more and more towards less wealthy countries, it is important that we tailor public health communication and solutions to meet the needs of the most affected communities.
We can learn a lot from the response to other disease outbreaks, where community-led solutions have helped to shape social norms and deliver important health interventions. For example, across Africa, innovative programmes have helped to control the transmission of HIV [PDF] by integrating testing with other healthcare services and by building local supply chains to deliver antiretroviral drugs.
Actively involving the communities who are most at risk in prevention and treatment efforts will be crucial to bringing Covid-19 under control and preventing future pandemics.

Read more about what we can learn from the 2014-16 West African Ebola epidemic to prevent future outbreaks.
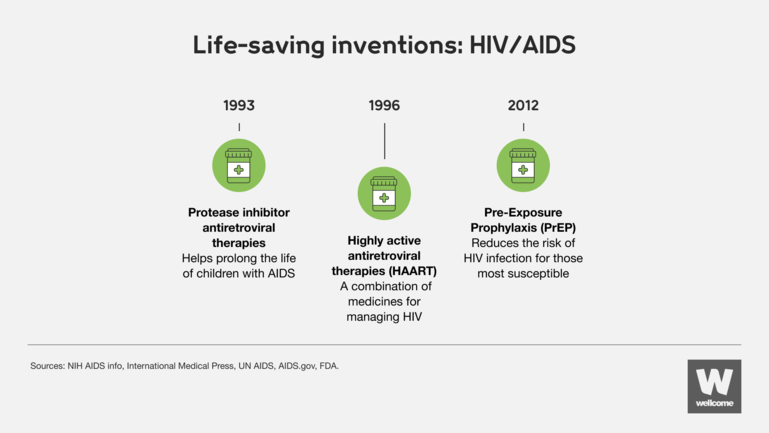
In the 1990s, former US president Bill Clinton decided to launch a bold new vaccine research centre in the hope of developing an effective HIV vaccine. Though unsuccessful in this mission, their research into mRNA vaccines was fundamental in creating the first approved Covid-19 vaccine 25 years later.
Likewise, the innovative PCR assay technology used to help monitor HIV patients in the height of the pandemic can now be found in the highly accurate Covid-19 tests that have been critical in controlling the spread of the virus.
The moral of the story? We can’t always know where the next life-saving science will come from.
The pace and innovation of Covid-19 research over the past few years has been staggering. It shows what is possible given the urgency, funding and political will of a global pandemic. However, many of the milestones in Covid-19 research sit on the shoulders of breakthroughs and developments years in the making.
As we work towards bringing the spread of Covid-19 under control, we cannot miss this opportunity to apply what we have learned to other deadly diseases, as well as prepare for future pandemics.
Whether making use of new public health facilities to improve access to HIV testing or trialling developments in mRNA technology to create a vaccine for HIV, there are already innovative, collaborative projects looking to the future of infectious diseases.
Over the next ten years, Wellcome plans to spend £16 billion to advance scientific discovery: from exploring the factors that drive infections to developing affordable medicines and diagnostics tools. The greatest opportunities for innovation in these areas will come from a diverse and collaborative community, combining strengths from many areas of research.
We’re funding research to better understand what causes and drives infectious diseases to escalate and the solutions to control their impact.
There are currently no open funding opportunities for Infectious Disease. Learn more about the funding we provide.