
How the response to Ebola outbreaks shows why we need to prioritise preparedness
Ebola is now a disease that can be diagnosed and treated. To prevent Ebola outbreaks from occurring in the first place, the world needs to be proactive to be better prepared. It can do this by prioritising community engagement, vaccination, filling research gaps and investing in infrastructure in high-risk countries.

Photo by John Wessels / AFP via Getty Images
What is Ebola?
In 1976, a new virus was discovered in what is now called the Democratic Republic of Congo (DRC). The disease, which killed many of those infected, was named after the nearby Ebola river.
Ebola is a zoonotic disease, meaning that it started in an animal host before spreading to humans. It is transmitted through direct contact with blood, body fluids, or contaminated clothing and other personal items of symptomatic or deceased patients or animals.
Without treatment, the average case fatality rate of Ebola is around 50%.
A vaccine candidate was developed in 2005, but a failure to prioritise epidemic preparedness and research meant that important safety trials, which can be done at any time, were not completed until the largest epidemic began nine years later.
Learnings from the 2014-16 West African Ebola epidemic
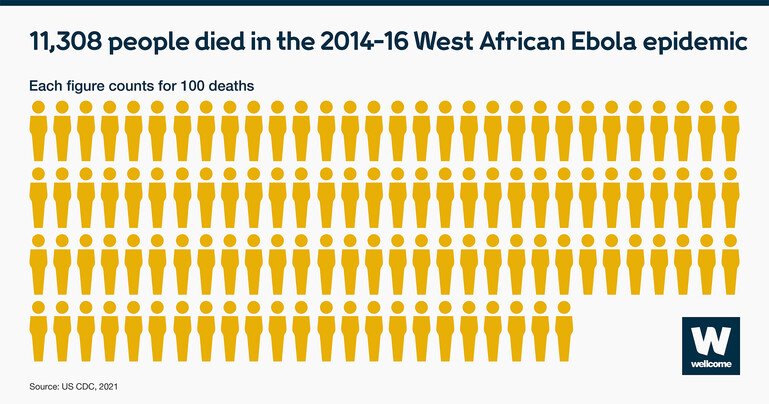
The West African Ebola epidemic of 2014 resulted in more than 28,000 suspected cases and 11,000 deaths. At the time, there were no vaccines and no treatments to help combat the disease. Because the amount of virus present in the body is known to be highest at point of death, traditional funeral practices – which include washing and touching the corpse – led to many people becoming infected in the earlier stages of the epidemic.
This epidemic was the catalyst for prioritising critical research to have better tools to prevent and respond to Ebola.
First, aid workers and researchers worked with the communities that adhered to traditional burial practices to negotiate slightly different practices. This made sure that future burials and funerals were medically safe but still acceptable to the community. Burial teams made up of local volunteers, gained the trust of the communities, which was critical to success.
Second, research took place on the frontline to help contain outbreaks. In response to the outbreak, public health officials and the pharmaceutical company Merck fast-tracked rVSV-ZEBOV, a single dose experimental Ebola vaccine. After a highly successful field trial in 2015, and further use to contain outbreaks in DRC in 2018, the US and EU regulators approved the vaccine in 2019. A second two-dose vaccine developed by Johnson & Johnson was given the green light in Europe in 2020.
However, while enhanced community awareness of how to tackle Ebola, vaccines and improved surveillance has proved successful at ending the spread of infection, new outbreaks continue to occur.
Ebola outbreaks in 2021 and 2022
Genomic sequencing of the virus from the most recent Ebola outbreaks suggests that they were a result of persistent infection of a survivor of earlier outbreaks, and not as a result of a new introduction of the disease from an animal reservoir. This highlights the need for preventative vaccination campaigns in areas which have previously seen Ebola outbreaks.
However, current Ebola vaccines are only licensed for the Ebola Zaire species of virus.
The 2022 Ebola outbreak in Uganda is the Ebola Sudan species of the virus, for which there is no approved vaccine. This is why to try to control the spread of the virus, health officials in Uganda are focused on contract tracing, improving access to, and speed of, testing and most recently, declared a three-week lockdown in the Mubende and Kassanda districts.
While we don’t fully understand the factors leading to new Ebola outbreaks, more can be done to protect those most at risk in Ebola-prone areas.
What to prioritise to be better prepared
1. Community engagement and education
Community engagement and social mobilisation are central to effective preparedness. Response teams must work with the community, religious leaders, journalists, radio stations, and partner organisations to build awareness of Ebola and community confidence in the tools that combat an outbreak.
2. Widespread surveillance and monitoring systems
Reinforcing disease surveillance across high-risk countries will help prevent any chance of a surprise resurgence. This requires a combination of a well-trained healthcare workforce with knowledge of the symptoms to identify, and the laboratory facilities to confirm the presence of the virus.
3. Prioritising filling the research gaps
Critical research is required to help better prevent and respond to Ebola outbreaks in the future. These gaps have been highlighted through a global consultation with researchers, public health institutes, and at-risk countries and outlined in the draft World Health Organization R&D Roadmap for Ebola and Marburg.
It should be noted that current Ebola vaccines have been developed to target and protect against one type of Ebola virus. But we know that there are other Ebola virus species that cause outbreaks – like the Ebola Sudan species. We need to invest in research to develop new Ebola vaccines to target these species. We also need to invest in research to develop new generations of Ebola vaccines to target any new variants that emerge.
4. Prevention-led vaccination strategies
Immediate response to outbreaks is critical to their containment. Proactive vaccination strategies in high-risk areas for Ebola could help curb the spread, and support the ‘ring vaccination’ approach – vaccinating healthcare workers and those in close contact with Ebola cases – to stop the virus from spreading.
All of these strategies require funding. From the provision of millions of vaccine doses, to the infrastructure and training to deliver them. But without global investment in these areas, we will continue to see outbreaks.
And Ebola is also far from the only deadly virus that humans face. In 2018, measles killed more than 140,000 worldwide, and influenza is estimated to result in about 3 to 5 million cases of severe illness, and about 290,000 to 650,000 respiratory deaths according to the World Health Organization.
We must invest in prevention and strengthen health systems, not just reactive responses, to stop an infectious disease outbreak turning into a deadly epidemic.
We’re funding research to better understand what causes and drives infectious diseases to escalate and the solutions to control their impact.
There are currently no open funding opportunities for Infectious Disease. Learn more about the funding we provide.

