
Apply for mental health research funding
We're funding research into digital, biological, psychological or social markers for mental health to ensure that people can get the right treatment at the right time.
John Torous and his team of clinicians, data scientists and app developers don’t look like your usual research team. But out-of-the-box thinking, as he explains, might be exactly what’s needed to find digital markers that can help take on some of the biggest challenges in schizophrenia research.

Towfiqu Barbhuiya / EyeEm via Getty Images

Assistant Professor of Psychiatry, Harvard Medical School

Assistant Professor of Psychiatry, Harvard Medical School
When I was training in psychiatry, it was always tricky seeing patients in the emergency department. We would try to understand their situation as quickly as we could, but you are often working to make the best decision with limited information.
Then one day a patient came in and it sounded like something very bad had happened in a personal relationship. The patient agreed to let us read their text messages and immediately it was very clear what was happening.
It was an eye-opening moment for me – to see how much information phones may hold to help guide mental health treatment, especially in schizophrenia.
The way that we understand schizophrenia is largely based on research study participants reporting on their own condition or circumstances – often quite infrequently.
This approach has enabled a lot of scientific advances, but we now know that every person has a rather different lived experience of the condition. People live in different environments, they have different stressors, and they experience different symptoms or changes over time.
There are three core types of schizophrenia symptoms:
It’s such a complex, dynamic illness that it has become nearly impossible to understand it using traditional measures and surveys. For example, there are still very limited methods for predicting relapse episodes, and whilst the cognitive symptoms of schizophrenia are often the most disruptive to people’s lives, they are the hardest to measure.
Yet we're still surprised when people end up back in hospital.
This limited understanding of schizophrenia has also stopped us from developing many new treatments or interventions.
Scientific advances start when we can measure and quantify what's happening. That’s why we need better measurements and tools for understanding schizophrenia. And that's where smartphones become so exciting.

We're funding research into digital, biological, psychological or social markers for mental health to ensure that people can get the right treatment at the right time.
Smartphones are incredibly powerful pocket computers.
They have very advanced sensors which can measure things like sleep, activity and heart rate, but they also have the ability to respond to these measures and actually deliver treatment. We learnt this during Covid-19, when doctors were able to schedule video call check-ins or use apps to send notifications.
What’s even more exciting is most people in the world have access to smartphones now. We don't have to give someone a complex medical device anymore or ask them to take time off work to come into the lab for a scan. The technology can also be easily shared and adapted to work across different cultures, languages and countries.
Ultimately, this makes smartphones an infinitely more scalable tool than existing methods.
But what does this look like in practice, what can you do with all this data once you’ve collected it and does it work in different countries too?
That’s what we’re investigating with our Wellcome-supported project, SHARP (Smartphone Health Assessment for Relapse Prevention), with a multidisciplinary team based across India and the US.
We have developed a mental health app called mindLAMP to understand when someone may be at risk of relapse in schizophrenia.
After securing the appropriate ethical permissions, we’re able to use mindLAMP to collect data from someone’s smartphone sensors. We can look at digital markers like geolocation, movement and screentime, or even send notifications to ask if they can take a survey on their phone.
We can then use these digital markers to predict when someone is not doing well by identifying anomalies in the data.
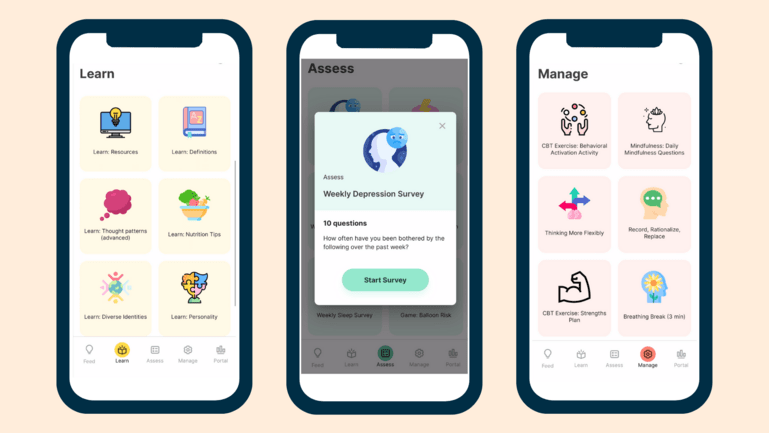
Previews of the mindLAMP app.
Division of Digital Psychiatry
The advantage of this approach is that we're looking at each person through their own patterns and their own phone. It's not perfect, but it’s certainly better than chance, and it's better than just asking people how they feel in a survey.
We were also able to adapt mindLAMP for different cultures and regions.
Working with our colleagues in India, we quickly learned that flexibility is very important.
The app has been designed in a modular system and is available and free to use for any researcher in the world. This means that clinicians and researchers can adapt the app to their own requirements: they can change the language and images, pick the sensors they want to use, write the surveys, add in education and activity elements – or include none of them.
It’s already been translated into Korean, German, Italian, French, Mandarin and Spanish, and used for everything from monitoring screen time in adolescence to managing cognitive symptoms.
We've probably been through over 100 updates to the app – most of them are driven by service users or patients.
It’s a unique challenge and requires a diverse team of people with a lot of different expertise – from engineers and data scientists to psychologists and mental health specialists. We certainly don't look like a traditional research team, but diverse teams bring in new ideas and perspectives, and challenge your ways of working.
We hope that the data mindLAMP can collect will continue to advance new discoveries in research for schizophrenia. Ultimately, our goal is that this could be translated into useful tools for a clinical setting.
Now that we know the app works, we want to see if smartphones can offer quick and easy tests that could tap into the different cognitive symptoms that affect people with schizophrenia (like attention, memory or problem-solving). For example, we could use it to see if a new medication improves cognition or if a relapse episode impacts someone’s problem-solving.
The role of technology in all healthcare is going to continue to increase, especially in mental healthcare.
As the two worlds begin to merge more, I think it will become standard to have teams with very different experiences and perspectives; bringing together people with UI and UX design experience, data scientists, patients, researchers and ethical specialists, all working towards the same goal. It’s a very exciting prospect to me.
We’re funding research to help create transformative change in early intervention for anxiety, depression and psychosis.
There are currently no open funding opportunities for Mental Health. Learn more about the funding we provide.
Tags


A monthly round up of stories about the research we fund and the global health issues we care about, delivered straight to your inbox.