Could Covid-19 be fuelling drug resistance?
We need to understand the impact of Covid-19 on wider health issues to shape better public health responses and limit long-term consequences. Drug resistance is one of these, Gemma Buckland-Merrett explains.
As the world continues to grapple with the Covid-19 pandemic, the impact of this crisis is already being felt across many public health issues.
We have seen routine immunisation paused, cancer screenings delayed and depression levels rise.
One of the most worrying wider health impacts could be the rise of drug-resistant infections – which public health experts have been warning for decades.
Many are concerned that Covid-19 may be fuelling this trend.
How Covid-19 could be accelerating drug resistance
1. Stretched healthcare systems
Prior to the pandemic, many hospitals were working hard to implement diagnostic and antibiotic stewardship programmes to avoid inappropriate use of antibiotics and ensure effective patient care. These protocols include taking blood cultures to confirm a diagnosis before prescribing patients with antibiotics.
Reports from some hospitals have found that during the early stage of the crisis, these diagnostic protocols could not always be followed or monitored as stringently as they were before the pandemic. So some patients will have received antibiotics unnecessarily, while others will not have received the most appropriate treatment for their infection.
2. Increased use of antibiotics
Although antibiotics are not effective against viruses, healthcare providers are advised to prescribe them for seriously ill Covid-19 patients to prevent and treat dangerous secondary bacterial infections. However, there are reports that patients with mild coronavirus symptoms have also been prescribed antibiotics in some hospitals.
A review of Covid-19 cases, mostly in Asia, found that more than 70% of patients received antimicrobial treatment, despite less than 10% having a secondary bacterial or fungal infection. The same study found frequent use of broad-spectrum antibiotics – designed to kill a wide range of bacteria – which can spur drug resistance if used too often.
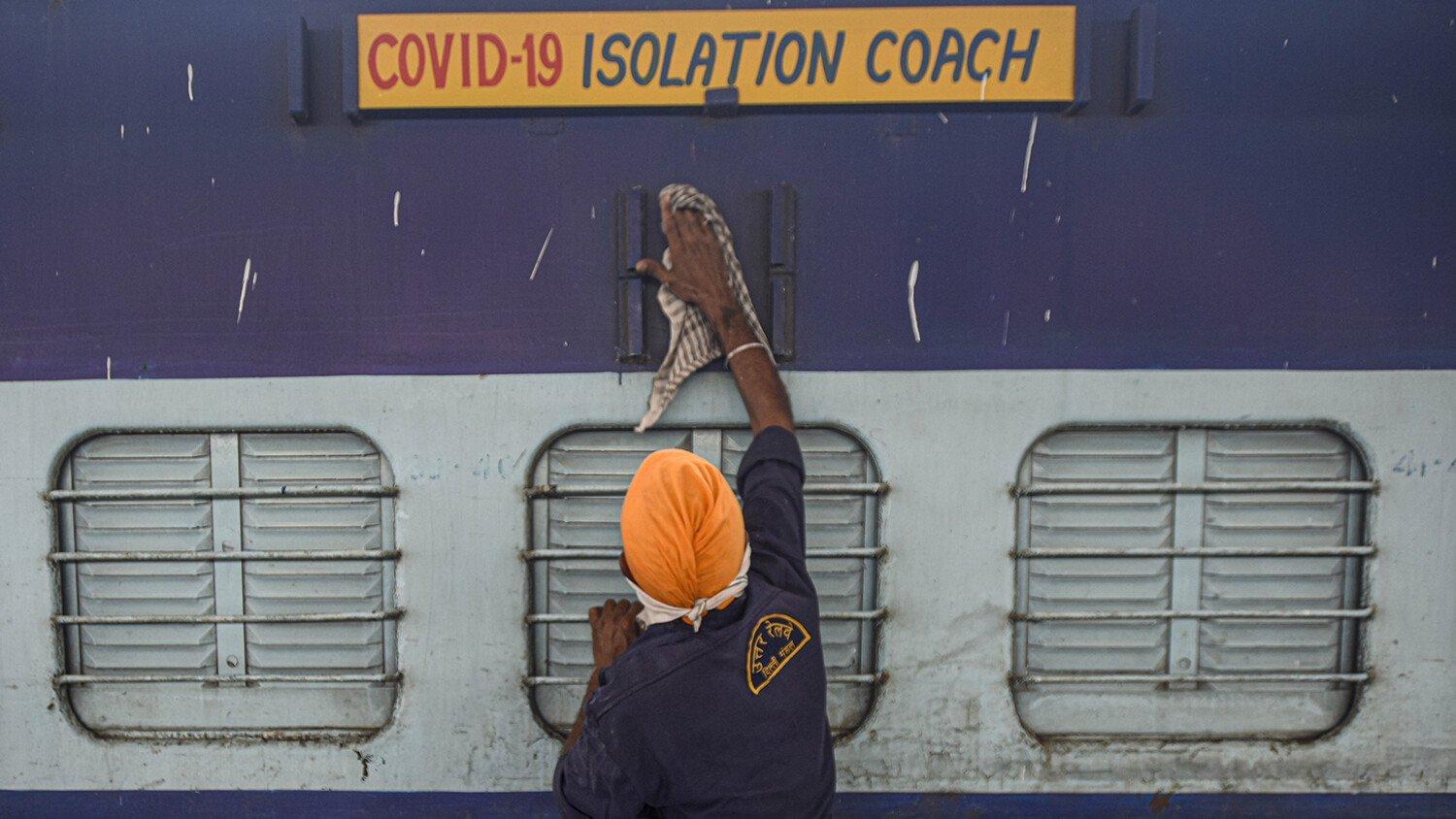
3. Changes to infection prevention and control in hospitals
The spread of Covid-19 has heightened societal awareness of personal hygiene and environmental contamination, but some hospitals have had to relax certain measures that prevent the spread of drug-resistant infections.
Measures such as the clustering of non-coronavirus patients in smaller wards could have unintended consequences by facilitating the spread of drug-resistant infections.
We need data and evidence to make better decisions
Early evidence and anecdotal accounts suggest that, since the pandemic started, there have been changes in hospital practices and an increase in antibiotic use – but has drug resistance risen as a result of these?
Wellcome is funding a large-scale study across hospitals in 11 countries to answer this question.
This cohort study, run by the University of Oxford, will use clinical patient data from a global network of hospitals, including some in countries significantly hit by coronavirus such as Italy, the UK, India, Iran, South Korea, Bangladesh, Nigeria and Brazil.
The study will seek to answer if there have been changes in adherence to diagnostic stewardship protocols, antibiotic usage, and infection control practices during the pandemic, and if there has been any major change in drug resistance as a result.
This research will provide the evidence base we need to better respond to the changes brought by Covid-19 and design appropriate interventions to limit the spread of drug-resistant infections.
Using data to guide public interventions and decision making is pivotal not just for pandemics, but for tackling all infectious diseases, including those that are becoming resistant to antibiotics and other drugs. Accurate antimicrobial resistance data is crucial for guiding patient care – ensuring that patients are getting the right treatment – and also for guiding public health decision making at a national, regional and global level.
Knowing the burden of drug resistance can help us make better decisions, such as which drugs to prioritise in development and which countries need support. But the surveillance systems, infrastructure and skills required to collect and use data are either non-existent or in bad shape in many low-resource countries.
This is why Wellcome has made the use of accurate data a central part of our work on drug-resistant infections. As well as funding studies like the one above, we have funded SEDRIC, a think tank that promotes the use of data to tackle drug-resistant infections. And we have forged unique public-private research collaborations with organisations like Pfizer Inc. to generate and use data sustainably in Ghana, Kenya, Malawi and Uganda.
These partnerships are making good progress, but more work is needed to set in place systems to gather, generate and use data around the world. If you have any ideas about this, we’d love to hear them. Contact us at drugresistantinfections@wellcome.org.