Episode 5: Can new technology help predict psychosis?
Alisha is in discussion with Professor Iris Sommer to understand more about psychosis – one of the most severe and stigmatised mental health conditions – and hear about an innovative AI project that could help us spot the signs early on.
Listen to this episode
Speakers: Iris Sommer, Alisha Wainwright, Tammy Tiba, Alexandre Loch
Iris Sommer 00:03
“We understand so little of the human mind, and then psychosis is such a challenge, which makes it fascinating, you know.”
Alisha Wainwright 00:13
Welcome to When Science Finds a Way – a podcast about science that’s changing the world. I’m Alisha Wainwright. And I’ll be meeting people with lived experience of our greatest health challenges – as well as the scientists and researchers working to make a difference.
Because not understanding what that lived reality is like, can lead to so much misunderstanding. And that’s especially pertinent for this episode, because we’re talking about psychosis. It might be a word you’ve heard before. But do you really understand what it means? Or can you think about it without just thinking about the stigma that surrounds it?
Tammy Tiba 00:58
“I was laying down in my bed and started hearing voices. I heard, ‘name of Father, Son and Holy Spirit’, something like that.
Alisha Wainwright 01:10
That’s Tammy. She’s going to share her story with us. And I’m also about to introduce you to Professor Iris Sommer, a global expert on psychiatry from the University Medical Center Groningen, in the Netherlands. She’s dedicated her career to understanding psychotic disorders – and how gender affects how we diagnose and treat them.
Iris Sommer 01:32
“Women have very different bodies, have very different minds, and they also experience very different stressors and different types of trauma.“
Alisha Wainwright 01:42
Speaking to Iris helped me feel more informed to talk about psychosis in a more inclusive way. As you’ll hear it’s something which I’ve witnessed in my own life, and if I’d known Iris back then, I’d have had a better toolkit for understanding it.
And what’s really exciting is that new research, using AI, COULD transform how we approach the condition. Does technology hold the key to preventing psychosis – the most misunderstood and stigmatised of all mental health disorders? We’re going to talk about that too.
There’s so much to discuss, so let’s get into it. Firstly, I asked Iris to help break down what psychosis actually is.
Iris Sommer 02:33
So, psychosis is a cluster of symptoms that makes you lose touch with reality. So others cannot really follow what you're worried about. It can be hallucinations, which means hearing, feeling, seeing things that others don't perceive. But importantly, it also has these strong convictions that others don't share with you. So for example, it can be the strong conviction that you're, that you're being followed by others that, that mean you harm, that can be very dangerous, or the strong idea that the water is toxicated, and that you're catching a severe disease by drinking it. Things like that, and convictions that are not easily changed with arguments, or even with evidence that it's not true. So this combination can be very frightening, can also be very lonely. And there are some cases in which it's not that bad. It can be friendly, but these are really few.
Alisha Wainwright 03:43
We've all probably heard the words psychosis and schizophrenia, but can you just explain what distinguishes them because people often use these terms interchangeably. But are they actually different things, right?
Iris Sommer 03:55
Yes, that's a good question. It's not the same but we tend to use them as if they are. At the start of psychosis, there's often other symptoms, which may be best summarised as a lack of energy, lack of motivation, and lack of ambition. That's what we call negative symptoms. And often it's a combination of the two. It's not only psychosis, but also the negative symptoms. And that combination is what we call schizophrenia spectrum disorders.
Schizophrenia has a kind of negative ring to it. This abbreviation schizo makes you think like there's something split – like maybe split personality or something. And that has nothing to do with the actual disorder it stands for. Some people also think that schizophrenia is a very severe disorder. Well, it can be but not necessarily. There are also cases of people who recover well from schizophrenia. So we tend to use the word psychosis as a kind of stand-in because it sounds more neutral.
Alisha Wainwright 05:02
Right, so schizophrenia is more than just psychosis. Do we have an accurate global picture of how many people are experiencing psychosis worldwide?
Iris Sommer 05:11
Yes, so psychosis is not really a diagnosis. So it's sometimes circumscribed as psychosis occurring with schizophrenia, but also with bipolar disorder, and also with let's say, major depression. And if you take those three disorders together, and add up every everybody who experiences psychosis, you will be somewhere around 3% of the population.
Alisha Wainwright 05:39
So, let's hear from someone with firsthand experience of this. Tammy Tiba lives in San Paulo, Brazil. She's now a director at a publicity agency but, 12 years ago, she experienced a huge change in her mental health.
Tammy Tiba 05:58
I started walking through the house here alone. I was laying down in my bed and started hearing voices. I was religious at the time. So I heard something like, ‘name of Father, Son and Holy Spirits’, something like that. I couldn't sleep well. I couldn't eat as well. So I lose weight. I was very thin, and my mom took me to the hospital. And the doctor said, I could have anorexia. But it wasn't a lose weight symptom, but it was in my mind. In the next four years, I was going to the hospital, but they didn't know exactly what one was. I couldn't work anymore. I couldn't study. I couldn't do the things that I used to do before the first episode. After four years, they diagnosed me with schizophrenia. And for me it was shocking. I kept a secret for a long time because there is, there is a stigma here. Even my, my closest friends didn't know until last year. My mum didn't tell about my illness to, to my relatives to… Since then, with the right diagnosis and treatment, I can do normal things like work, like going out with friends. I am very well now.
Alisha Wainwright 08:04
Wow, four years, it took Tammy four years to get a diagnosis, which in her case was schizophrenia. How hard is it to get a diagnosis with these conditions?
Iris Sommer 08:15
Well, I think the fact that she's a woman has added to this long time waiting. Because, especially for for a young man, the the picture of psychosis, sometimes together with, for example, cannabis abuse is quite typical and usually well recognised. But for women, you often see a misdiagnosis, like in her case, anorexia. Women are treated, but usually for depression. And it may take some additional years until until the psychotic symptoms are also evaluated, and also treated. This is a thing that we can still improve to shorten the duration of untreated psychosis. That's how we call it, especially for for women.
Alisha Wainwright 09:01
Well, Tammy also talked about stigma that she and her family felt once they got the diagnosis. I mean, how common is this? And how does stigma form part of the problem too?
Iris Sommer 09:12
It is, yes. There’s stigma, also self-stigma, people can be very ashamed of their symptoms, because it can be a bit unpredictable. So if you don't really understand what's going on in somebody else's mind, it can be frightening for others, which may make people avoid them. There is a lot to do about stigma. But I think really the best way to fight stigma is to treat psychosis. Because once psychosis is treated, then people become predictable again, and they become understandable again.
Alisha Wainwright 09:49
Yeah, I've personally experienced in college, a friend who ended up experiencing psychosis mixed with other things. And I will admit that I too, had my perceptions affected by stigma. But it was scary, because she didn't make sense to me. And I think a lot of what I used to rationalise the situation is what made sense, and what didn't make sense. And if it didn't make sense, I didn't necessarily want to be around it, which probably didn't help her feel good either. So she probably internalised things further. So I can see how stigma can become a problem.
Iris Sommer 10:27
Yeah, that's a very good example. That's exactly what happens.
Alisha Wainwright 10:30
So she says she's better now, how common is that?
Iris Sommer 10:34
Well, actually fairly common. I'm glad that I can say that, because we often think that after psychosis, there's only, only bad things - that, that's luckily not the case. So there are quite a lot of people that at least initially do well, and also I think, maybe, maybe one quarter of them who remained doing fairly well. So that's nice that she's also an example of that, because this is also what happens after schizophrenia. Broadly about 1/3 of them will do well, 1/3 of them will do sometimes well, sometimes not so well. And 1/3, unfortunately, rather poorly. That is incorporating treatment.
Alisha Wainwright 11:16
So let's zoom out a bit. Why does psychosis happen to people? And what are the causes and risk factors?
Iris Sommer 11:24
Like most psychiatric disorders, it's a mixture of about as much vulnerability, which can be genetic and about half environmental factors. And of course, it differs per person. And there are several quite well known risk factors it starts already during pregnancy, if pregnant women have viral infections. Also, birth complications are a clear risk factor. And something as global as being born in the winter months, that's already a risk factor. We think it's related to viral infections, but that's not so sure. Then we have growing up in an urban environment, the larger the city in which you grow up, only in the early years, the higher the risk for schizophrenia. Childhood trauma is a very big factor, especially for hearing voices. Then bullying at school is also a risk factor. Drug abuse is yet another one. And then we're already in the teenage, early adolescence, and then it's lack of sleep, which is maybe not so much a risk factor, but more a trigger.
Alisha Wainwright 12:43
It’s interesting, because later in this series we’re going to hear more about the connection between sleep and psychosis, and meet a researcher who’s pushing to use sleep treatments as a primary intervention for people experiencing psychosis. What are the ways we treat people for psychosis at the moment?
Iris Sommer 13:02
There's some cases, but they are few, that will not need medication – that are just light and can go on with a lot of psychoeducation which means clarifying what's going on, including family, partners, other important persons. And what we typically add is cognitive behavioural therapy, and that's dialogue in trying to make a person see where the thinking process goes wrong. In most cases, medication is also needed, at least for a while. And that's what we call anti-psychotic medication. There are different types of anti-psychotic medication – they all have one thing in common, which is that they impact the dopamine receptor, specific type of the dopamine receptor.
Alisha Wainwright 13:57
Can you just describe what dopamine is, for those who might not remember from, from college classes?
Iris Sommer 14:03
Yes, it's one of the neurotransmitters. It has several functions, also for movement and for cognition, but what we're now talking about is giving importance to whatever happens around you. So if, for example, you ride your bike through a busy city, you will see so many things, hear so many things, smell, even feel so many things. And most of these things just need to be ignored, because it's way too much for your brain to notice them all. But some of them are really important. Like, for example, this cab running through red light, and that might knock you over, you really need to note that one, otherwise you’re history. But there are other signals like for example, neon lights, trying to sell you whatever they want to sell you - you can really better ignore them. Now, dopamine helps to make you pay attention to the important ones, while neglecting the non-important ones.
Alisha Wainwright 15:01
Got it
Iris Sommer 15:02
Okay. So if the regulation of dopamine is disordered, you may mistakenly give a lot of important to non-important things.
Alisha Wainwright 15:12
Like a neon sign trying to sell you something? Yeah.
Iris Sommer 15:15
Exactly. Exactly, and you may develop the conviction that this is a personal message telling you that you urgently need to go to, well, let's say some fast food restaurant to meet someone who's waiting there for you to save the world - something like that. So dopamine has this role. And what anti- psychotic medication is doing is suppressing that. 80% of persons actually do experience remission of psychosis with medication, which is good. That's really quite a high number. There are also some disadvantages, which is the side effects And they vary per medication. But there's no medication which really has no side effects at all, mostly patients do experience some side effects.
Alisha Wainwright 16:07
And does the side effects cause people to stop taking them?
Iris Sommer 16:11
It can, but there's also – antipsychotics have a stigma too. Sometimes people don't really experience them at that moment. But they're really afraid that they will cause side effects later on. There are some side effects that can be really severe. But even if they're absent, then people still really want to stop using them because they just have a very negative image.
Alisha Wainwright 16:36
Is there any evidence that it's possible to manage some aspects of psychosis, such as hearing voices, with talking therapies as an addition to, or instead of medication?
Iris Sommer 16:49
Yes, certainly. Treatment is not only medication, and at least where I work, in the Netherlands, it's usually a combination. So, sometimes people are hearing voices, and that's it, but it's no delusion. And then just psychotherapy may do the trick. And persons may not need anti-psychotic medication. In fact, for a person who doesn't have psychosis, and doesn't have the delusions, the convictions, I wouldn't say there is a need to prescribe anti-psychotic medication.
Alisha Wainwright 17:25
One of your research focuses is gender inequalities and the treatment of psychosis and schizophrenia. Can you explain your research a little bit more?
Iris Sommer 17:35
Yes, well, I think psychiatry has long suffered from, let's say, bikini vision. So all differences between the sexes are just breasts and sex organs, while they are also present in the brain, in the liver and the stomach, in the gut, in the blood – actually everywhere. So it's not one size fits all. And women have very different bodies, have very different minds, and they also experience very different stressors and different types of trauma. And they all affect diagnosis. The symptoms of psychosis just look differently in girls and women, compared to men. They also start usually at a much later age, but also treatment needs to be quite different. And for example, I was quite shocked when I was looking at pharmacotherapy. So that means anti-psychotic medication. When I just looked at something simple like concentration of those drugs in the bloods, then for some drugs, it was almost double the values of man, when women are dosed for the same. And we do tend to dose women similarly to man, and this really isn't good practice. So women have for awhile been excluded from drug trials, for good reasons, of course, to protect them. But this has created the knowledge gap that we really need to fill in very soon because it's quite clear that women should be treated differently for most psychiatric drugs, not only anti-psychotic drugs. We don't know what the optimal drug therapy for women is, let alone what happens during pregnancy and during menopause. So we knew that female hormones change a lot over menopause. And they will change liver function, acidity of the stomach, so many physiological functions. And that will also affect how much of the drug will be available in the brain. So we probably need to need to change dosing of anti-psychotic drugs, and other drugs as well. But we just don't know exactly how. Now, this is a huge knowledge gap that we need to fill as quickly as possible. It's not difficult. It's not rocket science. It's just, we're just lagging behind. It's just that –
Alisha Wainwright 20:01
It’s just brain science, yeah.
Iris Sommer 20:03
Isn’t it? Just something we need to do.
Alisha Wainwright 20:08
Yeah. Do we fully understand psychosis? Or is this an ongoing subject that is just continuing to be researched?
Iris Sommer 20:17
Yes, it's definitely the last. It's still very mysterious. We know a little bit. And it's, I think it's fascinating if, if I have the opportunity to talk somebody to talk to somebody who has psychosis, and I often do have that opportunity, then I'm always fascinated about how can this happen, what is happening, what's going on? And we understand so little of the human mind, and then psychosis is such a challenge, which makes it fascinating, you know. I've been researching it for 20 years, and I can definitely go on another 20 years before we really understand [a bit? 20:52] and it's so I think there's, I don't know 10,000 people researching psychosis and schizophrenia around the world and we still have so much to do. So this is definitely a field that we are just beginning to understand a little bit.
Alisha Wainwright 21:11
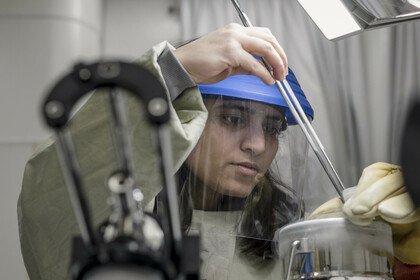
Well a really exciting research area where we’ve been seeing new developments around psychosis is the use of AI, and whether it can be used to spot the signs early on. I know that this is something you’ve been looking at Iris, and so has Dr Alexandre Loch. He’s a psychiatrist and associate professor at the University of Sao Paulo, and he’s been studying at-risk individuals since 2015. His team has developed an algorithm which analyses the speech, language and facial expressions of 18 to 30 year old participants, to detect whether they might be displaying the early signs of psychosis
Alexandre Loch 21:54
First, we ask about his or her childhood, how it was, their relationship with their parents, and we get the subject talking. And in a second moment, we show some pictures about a baby, a puppy and a dessert. And we asked the subject to tell a story about whatever comes in, in the mind about these pictures, we also ask about recent dreams, and also an old dream. So we've, we record this in a webcam, or in the mobile phone, usually. And then we got some data science guys who extract the video features. So it's basically to transform the facial expression and movement, is basically to transform this in numbers, then he has an AI machinery who reads these numbers and determines, let's say, who is healthy subject, and who is at risk. These at risk individuals would get some counselling. Okay, you might develop something in the future. So perhaps you should pay more attention to your mental health and do some psychotherapy. And this, this kind of stuff. We are able to intervene very early in the course of mental disorders.
Alisha Wainwright 23:16
So…. What do you make of this technology, Iris?
Iris Sommer 23:20
I really like this type of detection, I think it's, it's so nice, because it has very little burden for the participants, all you have to do is watch a video, make up some stories, this is really easy. You know, it doesn't involve drawing blood or being in an MRI scanner. I think this is so light and easily applied. I think it's very elegant, that exactly this method is chosen. And I can also see that it will be very informative.
Alisha Wainwright 23:52
So could this technology really help? He mentioned intervening early and recommending therapy? How important is this?
Iris Sommer 23:59
Well, that's the difficult part. I think the detecting part from this plan is great. I just love it. And I will watch this study with huge interest. But then what to do with the high risk group? That's difficult. And that's also from an ethical perspective, difficult, because there will be false positives in them also. So for some people, you may, you may actually worry them. And of course, you can't be 100% accurate. So –
Alisha Wainwright 24:31
Sure, that's the risk, right? The risk is that you might miss some people. Or you might tell some people that they're predisposed when they're not. And that could be pretty harmful.
Iris Sommer 24:42
Yeah, that's the risk you take. On the other hand, what can people really do if they will develop psychosis? So for example, we talked about sleep, so that's a good one. So I think it would be really helpful if you if you can tell people that are at high risk to develop psychosis, it would be very helpful to recommend them not to skip nights of sleep, and of course not to take drugs. But then, what about stress? You know, stress will find you whether you like it or not, you know? Like relations breakup, that's what happens to youngsters, it can be very stressful and it's difficult to avoid that. Preventing psychosis is a difficult thing, one way or the other. And it starts with detection. So detection is important. But I don't think the field really has figured out what to do with people that have been identified as high risk.
Alisha Wainwright 25:38
I understand. Yeah.
Iris Sommer 25:40
We talked about the duration of untreated psychosis. So the least thing we can do is early detection. So once psychosis is really present, then we can have an early treatment, which is also very important.
Alisha Wainwright 25:54
Yeah, I'm just thinking of, you know, Tammy, who we heard from earlier, if she had been diagnosed properly, she wouldn't have had to spend four years stressfully thinking about what was wrong with her. And there could have been a better medication plan, a better psychotherapy plan. And all of those things could have come into play had she been diagnosed properly, sooner.
Well, here's Alexandre’s vision for his algorithm, but also his thoughts on some of the ethical challenges around this technology.
Alexandre Loch 26:28
My dream with this research is that in the near future, we use this app like – it will be like a common app. We wouldn't fear mental disorders, we wouldn't have stigmatising beliefs about it. And we will use this app to make, let's say, a regular checkup, like, Okay, you go to the – your general practitioner to see if your health is good, to see your blood levels, your sugar levels, your cholesterol. Why don't we do this with mental disorders? Okay, I'm just recording here in my app and my phone, let's say five minutes of a free speech talk, talking about my life. And this app will upload the video and analyse it and give me a feedback. Okay, you're okay. Please go on. Or it seems that you're not okay. Please see a counselling centre, or seek a psychologist, and do some therapy or, I don't know, eat healthier or sleep better. If you tell people that this app is built by scientists, it was developed by universities and they are not trying to make you buy this, it is not an advertisement – this would be of much help for people to actually use the app. And secondly, if you could assure that it has many security layers and it's encrypted, and is that your video won't be used for, for anything else, this would also allow people to trust the app. So I think these are the basic issues that should be clear about the app.
Alisha Wainwright 28:11
Is that the future? Is that what we can kind of hope to expect – a future where you can just get a regular checkup at the doctor's?
Iris Sommer 28:20
Well, yes, and no, I love the idea of just using an app to aid diagnosis. I love the way he explains how it can reduce stigma; I much agree on that. But the part I don't agree with is that it should just be a general screening for everybody. I'm not sure if he's maybe, maybe he doesn't mean that. Because, it means that the chance for a false positive screening is high. But if you use an enriched sample, for example, people that are already visiting their general physician because of mental complaints, it would be much stronger, and that would largely reduce the false positive chats. And yeah, I think the general physician, or maybe a nurse physician, or maybe for younger people, even the school nurse, could be a very good venue to use this app, I think I'd rather see it in the hands of a clinician than just people downloading this, like we're doing was meditation apps, and just using it without any, any guidance.
Alisha Wainwright 29:27
Are there other ethical considerations that he should be keeping in mind?
Iris Sommer 29:32
Yeah, well, there’s lots of it. And I'm sure he has them in mind, as well. Because whatever we develop, for good use in clinical practice will also be used on the wrong location, you know. So if this app is freely available, of course, people in school will use it on their teachers or on their classmates or whatever –
Alisha Wainwright 29:53
Sure, I didn’t even think about that.
Iris Sommer 29:54
Those things happen.
Alisha Wainwright 29:55
Yeah, yeah
Iris Sommer 29:56
And how about data privacy? What if someone wants to take back his or her consent to use his data? Can you still find these data and take them out of the group? And what about hackers, can hackers somehow login to where you're storing the data? So there's, there's definitely a lot of ethical involvement in doing this type of research. And it's important to, to collaborate with people that, that are experts on that, also lawyers. But that doesn't mean that we shouldn't develop them, because I really see that this app will be very welcome and will have a very good place. Once we know exactly how accurate it is. And once we've figured out the steps to follow a positive screening, I think this will be a great new tool for clinical practice.
Alisha Wainwright 30:51
Tech can be biased as well. And are you fearful that with the already, you know, known biases that women experience in mental health diagnosis, for example, will we see a potential reflection of this in the technology being developed to help?
Iris Sommer 31:12
Yes, because, for example, voice recognition works better for male voices, because it's trained on more male voices, but it can be dealt with. So for example, if you want to analyse speech, which is an important aspect, if you want to have early recognition of psychosis, then it's important to make different algorithms – one for men and one for women. For example, pitch is completely different between men and women, and anxiety will be reflected in pitch. So, the female voice is already higher. So might be misclassified as anxious, you know, an anxious male voice may sound similar to a relaxed female voice, but just making different algorithms for male and female participants, and perhaps also for people with different cultural backgrounds – that will be very helpful.
Alisha Wainwright 32:14
What's your hope for the future of how we view and treat psychosis? And how could new technologies that we've heard about today play a part in that?
Iris Sommer 32:24
Well, for the near future, I think early detection is the way to go. Especially for female patients, reducing the duration of untreated psychosis, that's something that's really feasible, and I think will be at hand, but also improving access to good psychosis care, especially in places where there currently is none.
So there are many countries around the world, where it's just impossible to reach a psychiatrist at all, and where people with psychosis and with schizophrenia are not treated at all. And of course many countries – you yourself from United States, where people just cannot afford being treated for mental health, not even for severe disorders like like psychosis. And there are there ethnic inequalities as well. And I think eHealth can be very helpful there. The psychoeducation, the information, but also the cognitive behavioural therapy that we talked about, this could be given by eHealth, and that could even reach persons in places where there are no, no psychiatrists, and could also be given free of charge.
Alisha Wainwright 33:37
When you say eHealth, my interpretation of that is something you would access over the internet?
Iris Sommer 33:43
We think that chatbots are the future. And one of the professions that can be very well taken over by chatbots is actually my profession, psychiatry –
Alisha Wainwright 34:51
Oh dear!
Iris Sommer 33:43
There has been a study with a chatbot. And she actually did pretty good. So I don't have the most difficult profession, I'm afraid.
Alisha Wainwright 34:03
Don’t say that – I also, you know, I do argue whenever people talk about AI, it's your collective knowledge of your entire industry of very educated professionals that have given AI the tools to do its job. So there's a percentage of that AI that is your brain so –
Iris Sommer 34:23
That's very kind of you
Alisha Wainwright 34:25
Yeah don’t discount that. Don’t discount that at all. I mean, something that I'm reflecting on as, as you shared your thoughts is, maybe it's not so much about trying to prevent psychosis, because maybe that's something that's not preventable, but it's more about detecting it as early as you possibly can, and then having access to resources to mitigate some of the distressing symptoms that can impact your life.
Iris Sommer 34:54
So let's say a person does not have full blown psychosis, but is already hearing voices. And I think that's exactly what Tammy talked about in her interview. So that would be a very nice stage to start psychotherapy, which could probably also be done by a chatbot on a free downloadable app, I can imagine. So that's something that I would really like to see coming in, in the near future, and it doesn't have to take long. And then connect it to the beautiful app that my colleague from Sao Paulo is creating, I could really see that having very good influence.
Alisha Wainwright 35:33
Wow. Well, Iris, thank you so much for our in-depth conversation about psychosis and the recent developments in technology.
Iris Sommer 35:44
Well, thanks so much. It was a pleasure to talk with you, and thanks for the very important questions.
Alisha Wainwright 35:52
Thanks for listening to this episode of When Science Finds a Way. And thanks to Iris Sommer, Alexandre Loch, and especially to Tammy Tiba for sharing her story with us.
You know, I really thought the key to psychosis was prevention, but I think maybe that’s unrealistic. And these new technologies offer us some exciting opportunities to detect it early on, once we’ve worked through the ethical side of things. I’m also not afraid to say I’ve had to work through my own stigmas around mental health in my life, and this conversation has certainly helped remove some of the stigma I felt about psychosis and I hope it has for you too.
When Science Finds a Way is brought to you by Wellcome.
If you visit their website – wellcome.org – that’s Wellcome with two L’s – you’ll find a whole host of information about mental health, as well as full transcripts of our episodes.
Make sure you follow us in your podcast app to get new episodes as soon as they come out. And if you feel you learned something important or interesting, or you just want to support the podcast, spread the word and share it with people you know.
Next time, we’ll be hearing how community-led research projects are improving the lives of people living in informal settlements around the world.
When Science Finds a Way is a Chalk and Blade production for Wellcome – a global charitable foundation that supports science to solve the urgent health issues facing everyone.
Show notes
Psychosis is one of the most severe, and most stigmatised, mental health conditions. But what if technology could help us spot the signs early on? Could more accurate prediction help guide earlier intervention, to produce better outcomes for people at risk of psychosis? Alisha is in discussion with Professor Iris Sommer, a global leader in the psychosis field, to examine exactly where the understanding of the condition is, whether we’re approaching treatment in an equitable way, and how we can ensure earlier diagnosis and better treatment.
They hear from a therapist in Brazil, Dr Alexandre Loch, and his patient Tammy about how hard a diagnosis can be, and why it can often come too late to prevent the onset of severe symptoms. Alexandre also shares his innovative work using AI to spot whether someone might be at risk of developing psychosis, hinting at a potentially transformative breakthrough.
Meet the guest
Next episode
Around the world, roughly one billion people live in informal settlements. These communities are especially vulnerable to extreme weather events. Alisha speaks to Professor Karin Leder about projects in Indonesia and Fiji that are collaborating with local communities to address these challenges.
Transcripts are available for all episodes.

More from When Science Finds a Way

When Science Finds a Way: Our podcast
Our podcast is back with a third season, uncovering more incredible stories of how scientists and communities are tackling the urgent health challenges of our time.