Chapter 5: Attitudes to vaccines
This is chapter 5 of the Wellcome Global Monitor 2018
Read all chapters
Summary
- Globally, eight in ten people (79%) somewhat or strongly agree that vaccines are safe, while 7% somewhat or strongly disagree. Another 11% neither agree nor disagree, and 3% said they 'don’t know'.
- In high-income regions, there is less certainty about the safety of vaccines, with 72% of people in Northern America and 73% in Northern Europe agreeing that vaccines are safe. In Western Europe, this figure is even lower, at 59%, and in Eastern Europe it stands at only 40%. In low-income regions, the proportion of people who agree 'strongly' or 'somewhat' that vaccines are safe tends to be much higher at 80% or above, with highs of 95% of people in South Asia and 92% in Eastern Africa.
- In France, one in three people disagree that vaccines are safe, the highest percentage for any country worldwide.
- Despite relatively high levels of vaccine scepticism in some countries, 92% of parents worldwide said that their children have received a vaccine to prevent them from getting childhood diseases, while 6% said they did not, and 2% said they did not know. The highest percentage of parents who said their children did not receive a vaccine were Southern Africa, 9% and East Asia and Southeast Asia, 8%.
- In most regions, people who have high trust in doctors and nurses are very likely to consider that vaccines are safe. However, this is less true in Western and Eastern Europe.
- There is a clear positive relationship between overall trust in scientists, as measured by the Wellcome Trust in Scientists Index, and overall attitudes towards vaccines, though the relationship is strongest in high-income countries.
In this chapter:
- Introduction
- Awareness of vaccines
- Perceptions of the safety of vaccines
- Perceptions of the effectiveness of vaccines
- Perceptions of the effectiveness and safety of vaccines
- Factors related to perceptions of vaccine safety
- Perceptions of the importance of vaccines for children
- Did people report vaccinating their children?
- The relationship between trust in scientists and attitudes towards vaccines
- The relationship between trust in doctors and nurses and attitudes towards vaccines
- Conclusion
Introduction
Vaccines are a vitally important application of scientific research that save millions of lives worldwide every year.1,2 They reduce healthcare costs and are an integral part of public health policy.3 The central importance of vaccines to global health is why we devoted a question series in the Wellcome Global Monitor to understanding people’s attitudes towards vaccines around the world.
Vaccines are also one of the few medical interventions with which most people have personal experience, and as a result they are sometimes used as a proxy for trust in the broader health system. Although vaccines have always generated some anxiety among people,4 their uptake has generally been widespread enough that deadly diseases such as smallpox have been eradicated, and many other debilitating infectious diseases such as tetanus and cholera, diphtheria and polio have largely disappeared in many countries.
However, over the past decade or so, an increasing number of studies5,6,7 have documented a rising number of people in both high-income and low-income countries who seem to be losing confidence in some vaccines, to the point of choosing not to vaccinate their children.8 According to organisations such as the WHO and UNICEF, gains in the world’s fight against vaccine-preventable diseases are at risk. Lack of confidence in the safety and/or effectiveness of vaccines and the health system, shortages of health workers and supplies, depleted or destroyed health infrastructure, poverty and access difficulties (such as distance to the nearest clinic), all threaten to disrupt the effectiveness of vaccination programmes.9
The WHO has specifically identified vaccine hesitancy – which the organisation defines as 'the delay in acceptance or refusal of vaccines despite the availability of vaccination services' – as one of the top ten health threats to the world in 2019.10
Box 5.1: Main research topics addressed in this chapter
- How do people around the world feel about the safety, effectiveness and importance of vaccines, and how do these views vary by region and country, and by key demographics such as gender, age, education level, income level and urban/rural residence?
- How are attitudes to vaccines related to trust in science and in health workers?
- Do positive or negative attitudes towards vaccines translate into practical outcomes such as non-vaccination?
Wellcome Global Monitor questions examined in this chapter
The Wellcome Global Monitor includes a series of items on vaccines based on the questions asked in the Vaccine Confidence Project™.11
People were first asked if they had ever heard of the term 'vaccine' before (in their local languages). The following statement was read at the start of this section of the survey:
A vaccine is given to people to strengthen their body’s ability to fight certain diseases. Sometimes people are given a vaccine as [insert country equivalent term for a shot or an injection], but vaccines can also be given by mouth or some other way. Before today, had you ever heard of a vaccine?
After this question, those who had heard of vaccines were asked about the importance of vaccines for children, the safety of vaccines, and the effectiveness of vaccines, along the following lines:12
- Do you agree, disagree, or neither agree nor disagree with the following statement? Vaccines are important for children to have.
- After the response was given to this question, the following question was asked to determine the intensity of the response: Do you strongly (dis)agree or somewhat (dis)agree?
- The same questions were asked with reference to two other statements: Vaccines are safe. Vaccines are effective.
- Parents were asked if, to the best of their knowledge, their children received a vaccine that was supposed to prevent them from getting childhood diseases such as polio, measles or mumps (or the most common vaccinations in each country).
People’s decision not to vaccinate – for whatever reason – is not just a personal choice of risk-taking; it also poses a risk to others. Being vaccinated protects an individual from being infected themselves, and if enough people are vaccinated, it stops the disease from being spread to the larger population.13 This provides what epidemiologists refer to as 'herd immunity', or protection from the disease for the entire population, including people who cannot be vaccinated for medical reasons.
But for herd immunity to work, a large proportion of the population needs to be vaccinated. How large depends on how contagious the disease is. For example, approximately 90–95% of the population needs to be vaccinated against measles for herd immunity to work.14,15 For less contagious diseases such as polio, the vaccination uptake needs to be 80–85% of the population.16,17 For influenza, the figure is closer to 75% for vulnerable groups (very young children, people with chronic illnesses and the elderly).18,19 If enough people choose not to vaccinate and to rely on herd immunity for protection, outbreaks of preventable diseases become more common, as we have seen with the recent measles outbreaks in several countries, including the US, India, Brazil and Ukraine.20
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
Box 5.2: Recent measles outbreaks attributed to insufficient vaccination rates
According to the Centers for Disease Control and Prevention, in developing countries, approximately 1 or 2 in every 100 children with measles will die from the disease or its complications.21 UNICEF warned as recently as March 2019 that cases of measles around the world were surging to 'alarmingly high levels', led by ten countries that accounted for approximately 74% of the increase, and others previously declared measles-free.22 This is a source of serious concern for public health professionals, as measles is extremely contagious and it is estimated that around nine in ten people who are not already immune will become infected following exposure.23
Table 5.1: Countries with highest increases in measles cases between 2017 and 2018
| 2017 | 2018 | Percentage increase 2017-2018 | |
|---|---|---|---|
| Ukraine | 4,782 | 53,218 | 1,013% |
| Madagascar | 85 | 23,558 | 27,615% |
| Philippines | 2,409 | 20,758 | 762% |
| Brazil | 0 | 10,362 | N/A |
| Yemen | 2,101 | 13,622 | 548% |
| Venezuela | 727 | 5,668 | 680% |
| Serbia | 702 | 5,076 | 623% |
| Sudan | 665 | 4,978 | 649% |
| Thailand | 2,033 | 5,160 | 154% |
| France | 518 | 2,913 | 462% |
(Provisional monthly data reported to WHO, March 2019, annually). Number of confirmed cases.
Awareness of vaccines
About nine in ten people worldwide had heard of vaccines prior to this survey
Public confidence is an important factor in maintaining high vaccination rates. Therefore, much of the recent research on attitudes towards vaccines has focused on vaccine hesitancy – especially why people might refuse vaccines even when they are available. In 2015, the Vaccine Confidence Project™ launched a Vaccine Confidence Index (VCI)™ to measure the change in confidence over time. The Wellcome Global Monitor included questions based on the VCI™ to measure public trust in the safety, effectiveness, and importance of vaccines.
Before the full field implementation of the questionnaire in over 140 countries, it was tested in 10 countries (in local languages), partly to establish whether the terms used were broadly well understood and interpreted across countries and different socio-economic groups. One of the findings from the testing was that it is important to provide simple definitions of technical terms, to ensure that people understand what they are being asked about, and whether they have previously heard of the term.
Therefore, the first question about vaccines in the Wellcome Global Monitor defined the word vaccine, and then asked people about their familiarity with the term, as follows:
A vaccine is given to people to strengthen their body’s ability to fight certain diseases. Sometimes they are given a vaccine as a shot or an injection, but vaccines can also be given by mouth or some other way. Before today, had you ever heard of a vaccine?
Those who answered 'yes' were asked specific questions about the safety, effectiveness and importance of vaccines. At the global level, almost nine in ten people (89%) had heard of vaccines before the survey, with results relatively consistent across global regions. The findings show that in only 2 of the 18 global regions (Southern Africa and Southeast Asia) a significantly higher proportion of people say that they have not heard of a vaccine (54% and 26% respectively).
The results for Southern Africa need further investigation. For example, in the region’s most populous economy, South Africa, people in rural areas were less familiar with the word ‘vaccine’ than people in large cities/suburbs, at 37% to 49% respectively. However, in general, people seemed to understand what a vaccine does when shown the action of administering one, even if they did not recognise the word itself.
Chart 5.1: Awareness of vaccines by region

See the interactive version of this chart.
Perceptions of the safety of vaccines
People in high-income regions are less likely to agree that vaccines are safe, compared to people in low-income countries
In line with the VCI™24 questions, the Wellcome Global Monitor asked people around the world about their level of agreement with three key statements regarding perceptions of vaccines: 1) if they are safe, 2) if they are effective, and 3) if they are important for children to have. Overall, most people around the world 'agree' that vaccines are safe. Eight in ten people (79%) 'strongly' or 'somewhat agree' that they are safe, while 7% 'strongly' or 'somewhat disagree', 11% 'neither agree nor disagree' and 3% say they don’t know or have no opinion.
The Wellcome Global Monitor highlights deeper pockets of doubt about the safety of vaccines in certain regions and demographic groups. For example, people in several higher-income regions are among the least certain about vaccine safety. Only 72% of people in Northern America and 73% in Northern Europe 'agree' that vaccines are safe, and the figure is as low as 59% in Western Europe, and 50% in Eastern Europe.25
By contrast, an overwhelming majority of people in lower-income areas 'agree' ('somewhat' or 'strongly') that vaccines are safe. The highest such proportions are in South Asia, where 95% of people said they 'agree' that vaccines are safe, and in Eastern Africa, where the figure stands at 92%.
Chart 5.2: Perceived safety of vaccines by region
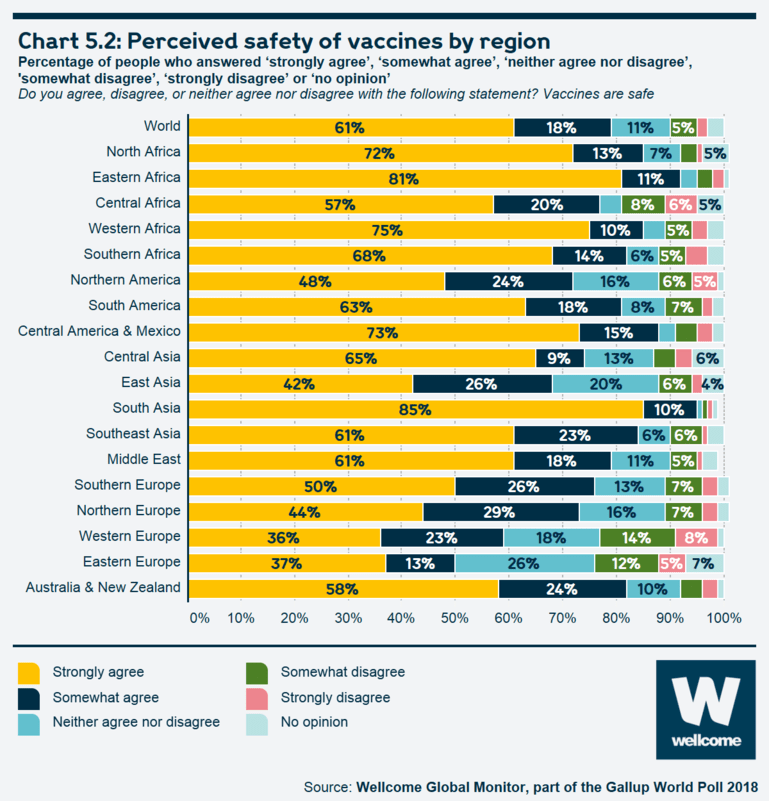
See the interactive version of this chart.
Perceptions of the effectiveness of vaccines
Eastern Europeans are least likely to agree that vaccines are effective
Worldwide, 63% of people 'strongly agree' and 21% 'somewhat agree' that vaccines are effective, or 84% who agree to some extent with this statement. Only 5% either strongly or somewhat disagree that vaccines are effective while another 12% either said they did not agree or disagree or said they had no opinion. Perceptions of the effectiveness of vaccines vary less by region than do views about vaccine safety. There are some significant differences, however, with Eastern Europeans being least likely to 'agree' ('strongly' or 'somewhat') that vaccines are effective, at 65%. Within Eastern Europe, the pattern is similar to the findings on vaccine safety, with countries that are in the EU having higher percentages of people who agree that vaccines are effective, compared to Eastern European countries that are outside the EU. For example, in Ukraine, only 50% of people 'agree' that vaccines are effective; this figure is 46% in Belarus, 49% in Moldova, and 62% in Russia. By contrast, three-quarters of people or more agree that vaccines are safe in Romania (75%), Czech Republic (76%), Hungary (78%), Slovakia (80%) and Poland (84%).
Chart 5.3: Perceived effectiveness of vaccines by region
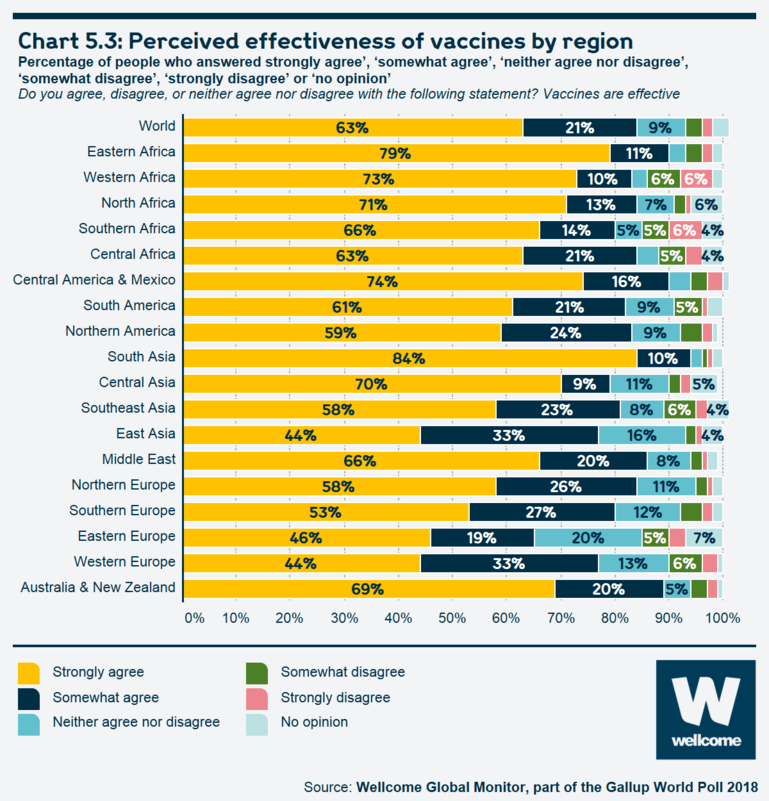
See the interactive version of this chart.
Perceptions of the effectiveness and safety of vaccines
Scepticism about vaccine safety does not always translate into scepticism about vaccine effectiveness
In several regions where people are least likely to agree that vaccines are safe, the percentage who agree that they are effective is significantly higher; the biggest gaps are seen in Western Europe (59% safe, 77% effective) and Eastern Europe (50% safe, 65% effective). This gap suggests that some people accept that they are effective at preventing certain diseases, even if they also believe some vaccines may have negative side-effects.26
Chart 5.4 highlights some interesting outliers. In Liberia, where 28% of people disagree that vaccines are effective (the highest in the world), just 3% of people disagree that they are safe. In a few other countries in sub-Saharan Africa, relatively high proportions of people disagree that vaccines are effective, though concerns about vaccine safety are less common. Liberia continues to grapple with infectious diseases such as yellow fever and tetanus, despite vaccination programmes.27 In countries where weak health supply and infrastructure systems exist, and there are difficulties with access to vaccines (in terms of distance to nearest clinics, for example), it is harder to achieve the vaccination rates necessary for herd immunity,28 and the persistence of infectious diseases may lead some people to conclude that the vaccines themselves are not working.
Chart 5.4: Scatterplot exploring people’s perceptions of vaccine safety and vaccine effectiveness
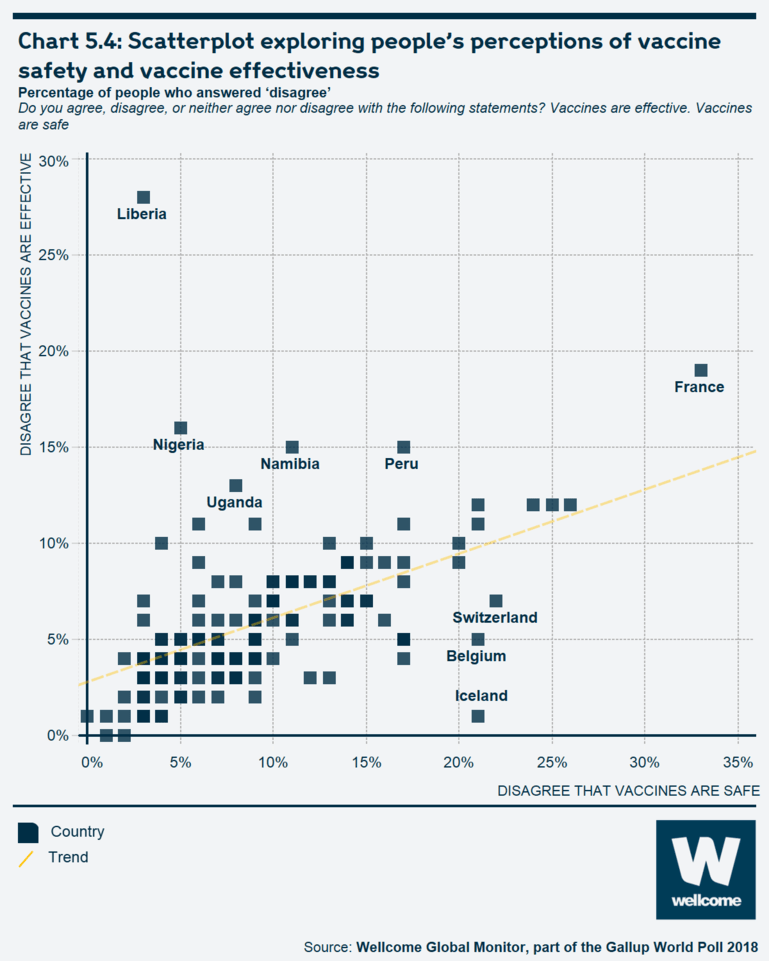
See the interactive version of this chart.
Box 5.3: Bangladesh and Rwanda: nearly universal agreement about the safety, effectiveness and importance of vaccines
Bangladesh and Rwanda are two of the most notable countries that achieve very high rates of agreement on all three items: vaccine safety, their effectiveness and the importance of children having them. In both countries, success in achieving very high immunisation rates was achieved despite numerous challenges in implementation.
In Bangladesh, the country’s strong commitment to childhood vaccinations is credited for achieving the Millennium Development Goal 4 of reducing childhood mortality.29 Since 2017, Bangladesh has also mounted vaccination campaigns with UNICEF and other agencies to halt the rapid spread of diphtheria and other preventable diseases among Rohingya refugees in the country.30
In Rwanda, according to the WHO, the country has seen tremendous success and progress in its vaccination programme over the past two decades. In 1995, the national immunisation coverage rate was less than 30% and incidence of vaccine-preventable diseases was very high. Over the past two decades, the authorities have adopted an approach that included working with international partners, local community health workers, and adopting technological solutions that could be adapted locally, in order to raise the immunisation coverage rate, which now stands at a remarkable 95%, with gender and geographic equity. The authorities have also successfully introduced six new vaccines into the routine immunisation programme, and the number of vaccine-preventable diseases has dropped significantly.
Table 5.2: Countries where people are most likely to agree that vaccines are safe, effective and important for children to have
Percentage of people who answered 'strongly agree' or 'somewhat agree' above 90%.
Do you agree, disagree, or neither agree nor disagree with the following statement? Vaccines are safe. Vaccines are effective. Vaccines are important for children to have.
important for children to have'
| 'Vaccines are safe' | 'Vaccines are effective' | 'Vaccines are | |||
|---|---|---|---|---|---|
| Strongly/somewhat agree | Strongly/somewhat agree | Strongly/somewhat agree | |||
| Bangladesh | 97% | Rwanda | 99% | Egypt, Ethiopia, Nicaragua, Northern Cyprus | 100% |
| Egypt | 97% | Bangladesh, Burundi, Cambodia, Colombia, Dominican Republic, Ecuador, Honduras, Iceland, Jordan, Nepal, Palestinian Territories, Rwanda, Sierra Leone, Tanzania, Venezuela | 99% | ||
| Ethiopia, Liberia, Tanzania | 96% | Bangladesh, Ethiopia, Iceland | 97% | Afghanistan, Argentina, Benin, Cameroon, Comoros, Costa Rica, Guatemala, Haiti, India, Laos, Malawi, Mexico, Myanmar, Sri Lanka, Uzbekistan, Zimbabwe | 98% |
| India | 95% | Afghanistan, Egypt | 96% | Brazil, El Salvador, Iraq, Kenya, Lebanon, Liberia, Madagascar, Mozambique, Nigeria, Norway, Tajikistan, Thailand, Uganda | 97% |
| Afghanistan, Rwanda | 94% | India, Tajikistan, Uzbekistan | 95% | Albania, Bolivia, Republic of the Congo, Gabon, Ivory Coast, Kosovo, Mauritius, Panama, Paraguay, Portugal | 96% |
Thailand, Sierra Leone, Uzbekistan, Venezuela |
93% | Cambodia, Comoros, Malawi, Thailand, Venezuela | 94% | Ghana, Peru, Senegal, Zambia | 95% |
| Jordan, Laos, Malawi, Mozambique, Nepal, Nicaragua | 92% | Myanmar, Norway, Sierra Leone | 93% | Botswana, Burkina Faso, eSwatini, Finland, Greece, Iran, Kuwait, Mali, Malta, Morocco, Namibia, Niger, Saudi Arabia, UAE, Uruguay | 94% |
| Malaysia, Myanmar, Nigeria, Palestinian Territories, Tajikistan | 91% | Dominican Republic, Jordan, Niger, Northern Cyprus | 92% | Chad, Denmark, The Gambia, Indonesia, Malaysia, Mongolia, Pakistan, Philippines, Sweden, Turkey, Yemen | 93% |
| Australia, Burundi, Republic of the Congo, Iraq, Laos, Madagascar, Mexico, Tanzania, Zimbabwe | 91% | Australia, Guinea, South Africa, Vietnam | 92% | ||
| China, Ireland, Mauritania, Netherlands, Tunisia, Togo | 91% | ||||
One in three French people disagree that vaccines are safe, the highest percentage worldwide
One of the most notable countries where a large percentage of people seem to be vaccine sceptics is France. Overall, one in three French people (33%) disagree that vaccines are safe – easily the highest proportion in the world. French people are also among the most likely to disagree that vaccines are effective, at 19%, and to disagree that vaccines are important for children to have, at 10% (see Table 5.3).31
Box 5.4: Why is vaccine scepticism so common in France?
The French are the most sceptical people in the world about the safety of vaccines, with one in three French people (33%) disagreeing that vaccines are safe. This level of scepticism is present and consistent across several demographic groupings within French society; it does not vary significantly by education, age, gender, urban or rural status, or whether people are parents.
Scepticism about vaccines in France is not new, but researchers noticed an increase after the controversial influenza pandemic vaccination campaign in 2009, during which the WHO was alleged to have been influenced by pharmaceutical companies.32 The rising vaccine hesitancy in France over the past several years – which even now includes some members of the medical community – has helped drive vaccine coverage among some children and young adults below immunity thresholds and led to rising numbers of measles and meningococcal disease cases.33
To help reduce this scepticism and combat rejection rates, the French government in 2018 expanded the number of compulsory vaccines from 3 to 11 for children up to the age of 2 years. In addition to the new law, the government is conducting promotional campaigns and providing additional support to healthcare professionals who have vaccine-hesitant patients. The mandate is intended to be temporary until the government sees evidence of higher confidence among the public.34
Chart 5.5: Perceived safety of vaccines in France by demographic breakdown
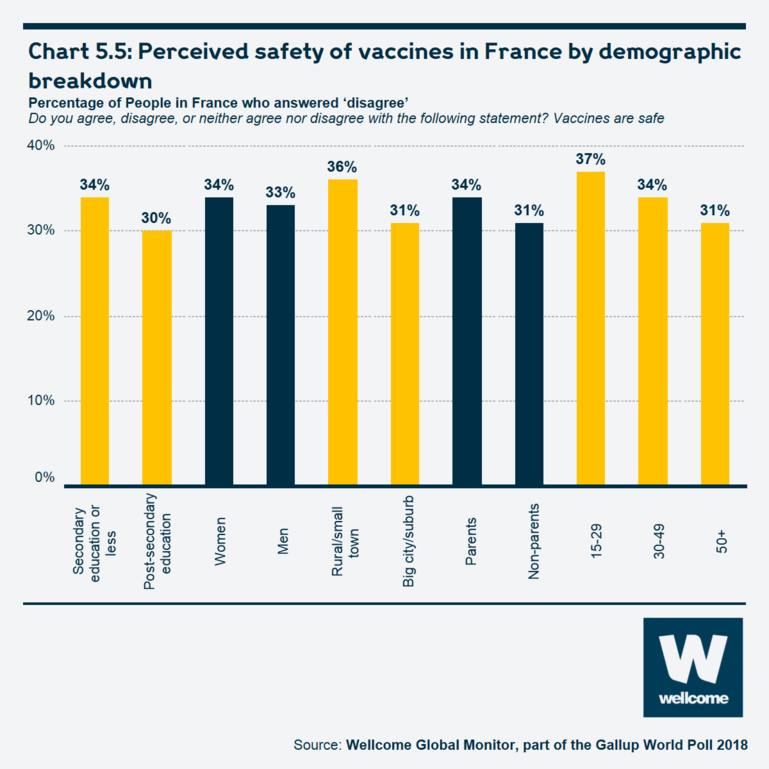
See the interactive version of this chart.
Table 5.3: Countries where people are most likely to disagree that vaccines are safe, effective and important for children to have
Percentage of people who answered 'strongly disagree' or 'somewhat disagree'.
Do you agree, disagree, or neither agree nor disagree with the following statement? Vaccines are safe. Vaccines are effective. Vaccines are important for children to have.
| 'Vaccines are safe' | 'Vaccines are effective' | 'Vaccines are important for children to have' |
|||
|---|---|---|---|---|---|
| Strongly/somewhat disagree | Strongly/somewhat disagree | Strongly/somewhat disagree | |||
| France | 33% | Liberia | 28% | Armenia | 12% |
| Gabon | 26% | France | 19% | Austria | 12% |
| Togo | 25% | Nigeria | 16% | France | 10% |
| Russia | 24% | Namibia | 15% | Russia | 9% |
| Switzerland | 22% | Peru | 15% | Switzerland | 9% |
| Armenia | 21% | Uganda | 13% | Azerbaijan | 8% |
| Austria | 21% | Armenia | 12% | Belarus | 8% |
| Belgium | 21% | Gabon | 12% | Italy | 8% |
| Iceland | 21% | Russia | 12% | Bulgaria | 7% |
| Burkina Faso | 20% | Togo | 12% | Moldova | 7% |
| Haiti | 20% | Austria | 11% | Montenegro | 7% |
| Indonesia | 11% | ||||
| Netherlands | 11% | ||||
| South Africa | 11% | ||||
Table 5.4: Perceived safety of vaccines by highest reported level of science education and region
Percentage of people who answered 'strongly disagree' or 'somewhat disagree'.
Do you agree, disagree, or neither agree nor disagree with the following statement? Vaccines are safe.
| Total | Primary level or did not study science or did not say | Secondary level | College or university level | |
|---|---|---|---|---|
| World | 7% | 7% | 8% | 10% |
| Central Africa | 14% | 11% | 16% | 17% |
| Southern Africa | 9% | 7% | 8% | 16% |
| Western Africa | 8% | 8% | 9% | 9% |
| Eastern Africa | 5% | 4% | 6% | 8% |
| Northern Africa | 4% | 3% | 5% | 4% |
| Northern America | 11% | 20% | 12% | 9% |
| South America | 9% | 8% | 10% | 10% |
| Central America and Mexico | 7% | 7% | 7% | 7% |
| Eastern Asia | 8% | 6% | 8% | 12% |
| Central Asia | 7% | 11% | 7% | 6% |
| Southeast Asia | 7% | 4% | 9% | 9% |
| Southern Asia | 2% | 2% | 2% | 2% |
| Middle East | 6% | 5% | 6% | 8% |
| Western Europe | 22% | 25% | 22% | 17% |
| Eastern Europe | 17% | 12% | 15% | 20% |
| Northern Europe | 10% | 13% | 9% | 7% |
| Southern Europe | 10% | 12% | 9% | 6% |
| Australia and New Zealand | 7% | 8% | 7% | 8% |
Factors related to perceptions of vaccine safety
Education levels influence confidence in vaccines differently in different regions
There is no obvious global relationship between levels of science education and vaccine confidence. In some places – like Northern Europe and Northern America – people with higher levels of science education are less likely to either strongly or somewhat disagree with the statement that vaccines are safe. In others – like Eastern Europe, Central Africa, and Southern Africa – the opposite is true. In places like South America, Central America and Mexico, and the Middle East, there is no significant difference between people with higher levels of science education.
Looking at the results by the type of area a person lives in – in or around a large city, a small town or a rural area – reveals that there are no significant differences, with the exception of Central Africa, where urban-dwellers are more likely than those in rural areas to disagree that vaccines are safe. This is the opposite to Western Africa and Western Europe, where rural dwellers are slightly more likely to disagree that vaccines are safe.
Table 5.5: Perceived safety of vaccines by type of area a person lives in and region
Percentage of people who answered 'strongly disagree' or 'somewhat disagree'.
Do you agree, disagree, or neither agree nor disagree with the following statement? Vaccines are safe.
| Total | Large city/suburb | Small town | Rural area | |
|---|---|---|---|---|
| World | 7% | 9% | 7% | 6% |
| Eastern Africa | 5% | 6% | 5% | 4% |
| Central Africa | 14% | 17% | 13% | 9% |
| Northern Africa | 4% | 6% | 1% | 3% |
| Southern Africa | 9% | 12% | 7% | 8% |
| Western Africa | 8% | 7% | 8% | 12% |
| Central America and Mexico | 7% | 8% | 6% | 8% |
| Northern America | 11% | 9% | 15% | 10% |
| South America | 9% | 10% | 8% | 9% |
| Eastern Asia | 8% | 9% | 8% | 8% |
| Central Asia | 7% | 7% | 9% | 6% |
| Southeast Asia | 7% | 8% | 7% | 6% |
| Southern Asia | 2% | 2% | 2% | 2% |
| Middle East | 6% | 5% | 7% | 7% |
| Eastern Europe | 17% | 19% | 14% | 16% |
| Northern Europe | 10% | 9% | 9% | 11% |
| Southern Europe | 10% | 10% | 9% | 11% |
| Western Europe | 22% | 20% | 22% | 25% |
| Australia and New Zealand | 7% | 7% | 10% | 7% |
People who recently sought information about science are less likely than those who did not to agree that vaccines are safe
The Wellcome Global Monitor asked people if they recently sought information about science or health, though it did not ask about information regarding vaccines specifically. People who recently sought science information are less likely to strongly or somewhat agree that vaccines are safe than those who said they did not recently seek information about science: 74% to 81% respectively. A similar result holds for recently seeking information about medicine or health (75% to 82%).
People who trust a doctor or nurse more than any other source of information are more likely to agree that vaccines are safe
The sources of information a person most relies on to find out about health matters is likely to be important in shaping individual perceptions. People who trust a doctor or nurse more than any other source of information (including friends/family, religious leaders, traditional healer or other) are more likely to strongly or somewhat agree that vaccines are safe than people who said they either trusted another source the most or did not name a source, at 72% to 81%. This relationship holds across all regions. This suggests that further research is needed in order to understand the link between attitudes to vaccines and sources of health information.
Box 5.5: Information sources and perceptions about vaccines
Anxieties and public concerns about the safety of vaccines have always existed, but the rise of social media has allowed the spread of what UNICEF calls the 'real infection of misinformation' to much wider audiences.35
For example, while a number of factors are likely to be behind declining vaccination coverage in Eastern Europe – where people are by far the least likely of any region to agree that vaccines are either 'safe' or 'effective' – some researchers claim that vaccine scepticism may have been bolstered by Russian disinformation campaigns that amplified the vaccine debate on social media. Researchers do not yet know enough about the influence of misinformation online towards intentions and behaviours in the region, and the WHO is hoping to shed more light on the relationship as it develops a framework on how to study vaccine hesitancy in the context of Russian and Eastern European culture.36
Perceptions of the importance of vaccines for children
Worldwide, 92% of people say vaccines are important for children to have
In general, people are more likely to say it is important for children to have vaccines than they are to agree that vaccines are safe or effective. Globally, 92% of people strongly or somewhat agree that it is important for children to have vaccines. This tendency holds in every region even among populations where scepticism about the effectiveness and safety of vaccines is most widespread, people are still more likely to say it is important for children to have vaccines. In Eastern Europe, for example, where just 50% of people agree that vaccines are safe and 65% agree that they are effective, 80% nonetheless say it is important for children to have vaccines.
However, some regional results for this question may still be a source of concern. Herd immunity for highly contagious diseases such as measles requires at least 90% of the population to be vaccinated, and for less contagious diseases such as polio, the required range is 80% to 85%.37 In that light, even if the 80% of people in Eastern Europe who agree that vaccines are important for children to have acted on their beliefs, it is still possible that the level of immunisation required for herd immunity for some diseases may not be met.
Within Eastern Europe, agreement is particularly low in Belarus (62%), Moldova (65%) and Bulgaria (71%).
Chart 5.6: Perceived importance of vaccines for children to have by region
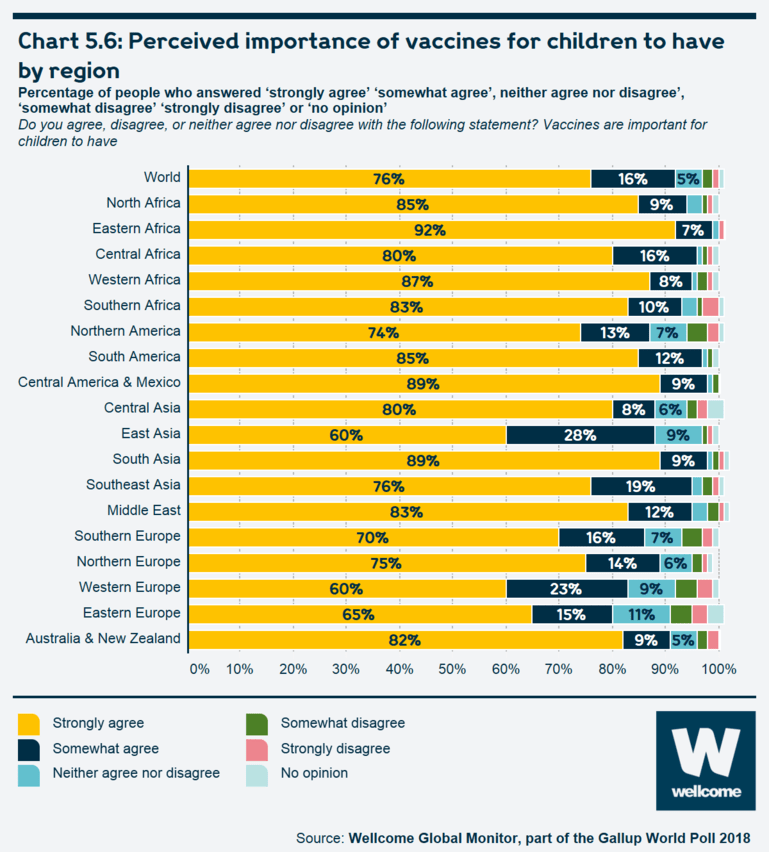
See the interactive version of this chart.
Some 92% of parents worldwide said that their children have received a vaccine to prevent them from getting childhood diseases, while 6% of parents said that they have not
Reflecting the high proportion who agree that vaccines are important for children to have, the vast majority of parents worldwide – 92% – said that to the best of their knowledge, one or more of their children had received a vaccine that was supposed to prevent them from getting childhood diseases such as diphtheria, polio or tetanus. In every region of the world, and regardless of income classification, at least 89% or of parents said one or more of their children had been vaccinated for such diseases.
However, globally, 6% of people said that their children did not receive a vaccine that is supposed to prevent them from getting childhood diseases. The highest percentages registered were in Southern Africa at 9%, as well as in East Asia and Southeast Asia, at 8% of people.
Chart 5.7: Map of proportions of people reporting vaccinating their children
Percentage of people who answered ‘yes’ by country.
To the best of your knowledge, have any of your children ever received a vaccine that was supposed to prevent them from getting childhood diseases such as diphtheria, polio or tetanus or not?38
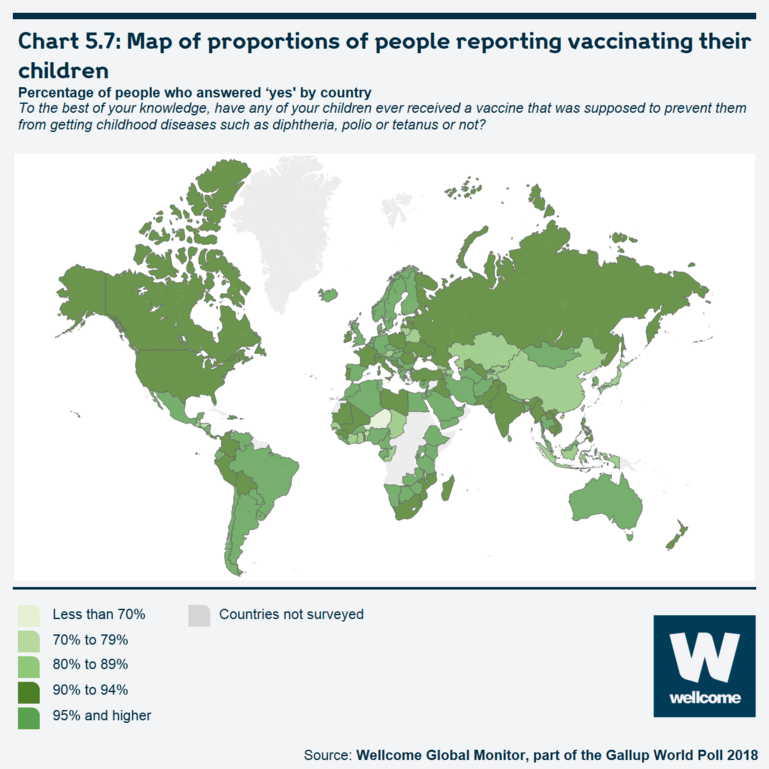
See the interactive version of this chart.
Did people report vaccinating their children?
However, there is more variation in these results at the country level; in 24 countries, less than 90% of parents say one or more of their children have been vaccinated, and in three countries, this number falls below 80% (see table 5.6). These are Honduras (77%), Benin (73%) and Niger (69%) – three countries, with relatively weak public health systems and a lack of resources to deliver sufficient health services, especially to people living in rural areas.
The presence of two high-income countries on the list – Japan and Austria – is notable. In the case of Japan,39 issues around the safety of the HPV and other vaccines in recent years have reduced public confidence in vaccines, and government policies over the past two decades have also been cited as a reason why there have been recent outbreaks of diseases such as rubella and measles.40 Also, contributing to the rise in the number of measles cases in the past year are the objections of some of the religious communities in the country to medicine in general, including vaccines.41
In Austria, it seems that an increasing number of people are choosing not to vaccinate out of fear of adverse effects, scepticism about the effectiveness of vaccines, and distrust towards the pharmaceutical industry.42
Table 5.6: Percentages of people reporting vaccinating their children by 24 countries with the lowest levels of reported vaccinating
Percentage of people who answered 'yes' by country.
To the best of your knowledge, have any of your children ever received a vaccine that was supposed to prevent them from getting childhood diseases such as diphtheria, polio or tetanus or not?
| Yes | No | Don't know/ refused | |
|---|---|---|---|
| Niger | 69% | 29% | 1% |
| Benin | 73% | 24% | 3% |
| Honduras | 77% | 19% | 3% |
| Lithuania | 82% | 4% | 14% |
| Georgia | 84% | 9% | 7% |
| Republic of the Congo | 85% | 14% | 1% |
| Tajikistan | 85% | 10% | 5% |
| Guatemala | 86% | 12% | 2% |
| Austria | 88% | 8% | 4% |
| China | 88% | 9% | 3% |
| Indonesia | 88% | 10% | 1% |
| Ivory Coast | 88% | 7% | 4% |
| Japan | 88% | 7% | 5% |
| Mauritius | 88% | 12% | 0% |
| Moldova | 88% | 8% | 4% |
| Armenia | 89% | 4% | 7% |
| Azerbaijan | 89% | 3% | 8% |
| Belarus | 89% | 3% | 8% |
| Chad | 89% | 10% | 1% |
| Ghana | 89% | 8% | 2% |
| Kazakhstan | 89% | 4% | 8% |
| Kyrgyzstan | 89% | 6% | 4% |
| Senegal | 89% | 8% | 3% |
| Taiwan | 89% | 10% | 1% |
The relationship between trust in scientists and attitudes towards vaccines
There is a positive relationship between overall trust in scientists and overall attitudes towards vaccines
There is a clear positive relationship between overall trust in scientists, as measured by the Wellcome Global Trust in Scientists Index (see Chapter 3) and overall attitudes towards vaccines, though the relationship is strongest among high-income countries. In particular, countries such as the Netherlands, the United States, the United Kingdom, Austria and New Zealand see large differences in perceptions of vaccines by overall level of trust in scientists, especially on the question about perceptions of vaccine safety.
Chart 5.8: Perceived safety of vaccines by level of Trust in Scientists Index among countries of different income levels
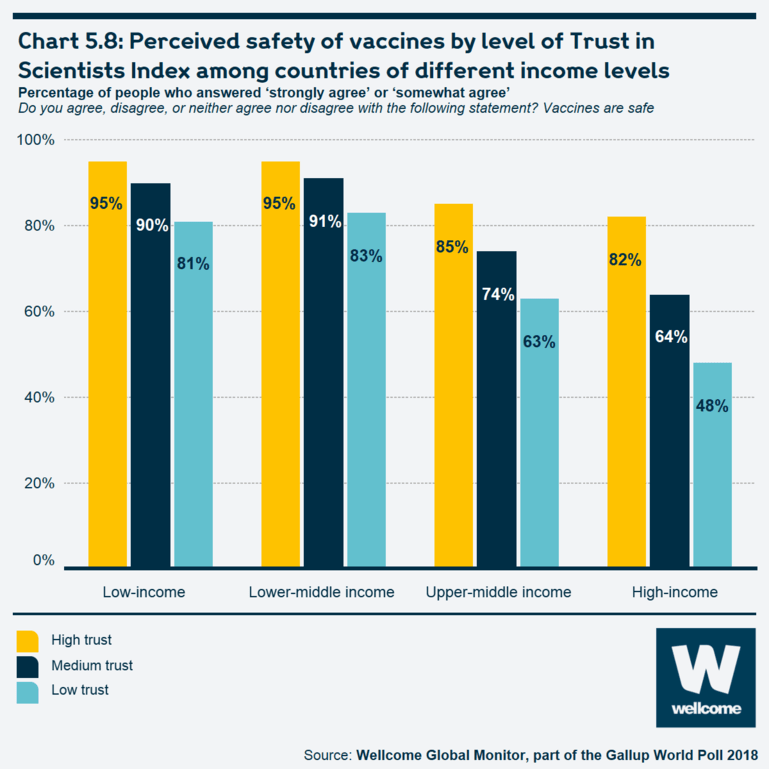
See the interactive version of this chart.
The relationship between trust in doctors and nurses and attitudes towards vaccines
People with a high trust in doctors or nurses are very likely to say vaccines are safe
In general, people are more likely to believe vaccines are safe if they trust scientists and medical professionals – though the relationship is strongest for trust in doctors and nurses. Worldwide, people who said they trust doctors and nurses 'a lot' are very likely to believe that vaccines are safe, at 87%.43 While high levels of trust in doctors or nurses are associated with high levels of agreement that vaccines are safe in all regions, this is less true in Western and Eastern Europe. In Eastern Europe, 67% of people who trust doctors and nurses 'a lot' believe vaccines are safe, perhaps due partly to the fact that in this region attitudes about various aspects of the healthcare system and healthcare professionals are comparatively less positive, including confidence in hospitals and clinics.
In Western Europe, slightly more than six in ten people who have 'a lot' of trust in doctors (63%) also believe vaccines are safe. Western Europe, however, has among the highest levels of trust in doctors and nurses of all regions, suggesting attitudes to vaccines are somewhat separate from overall healthcare perceptions.
Chart 5.9: Perceived safety of vaccines by level of trust in doctors and nurses and by region
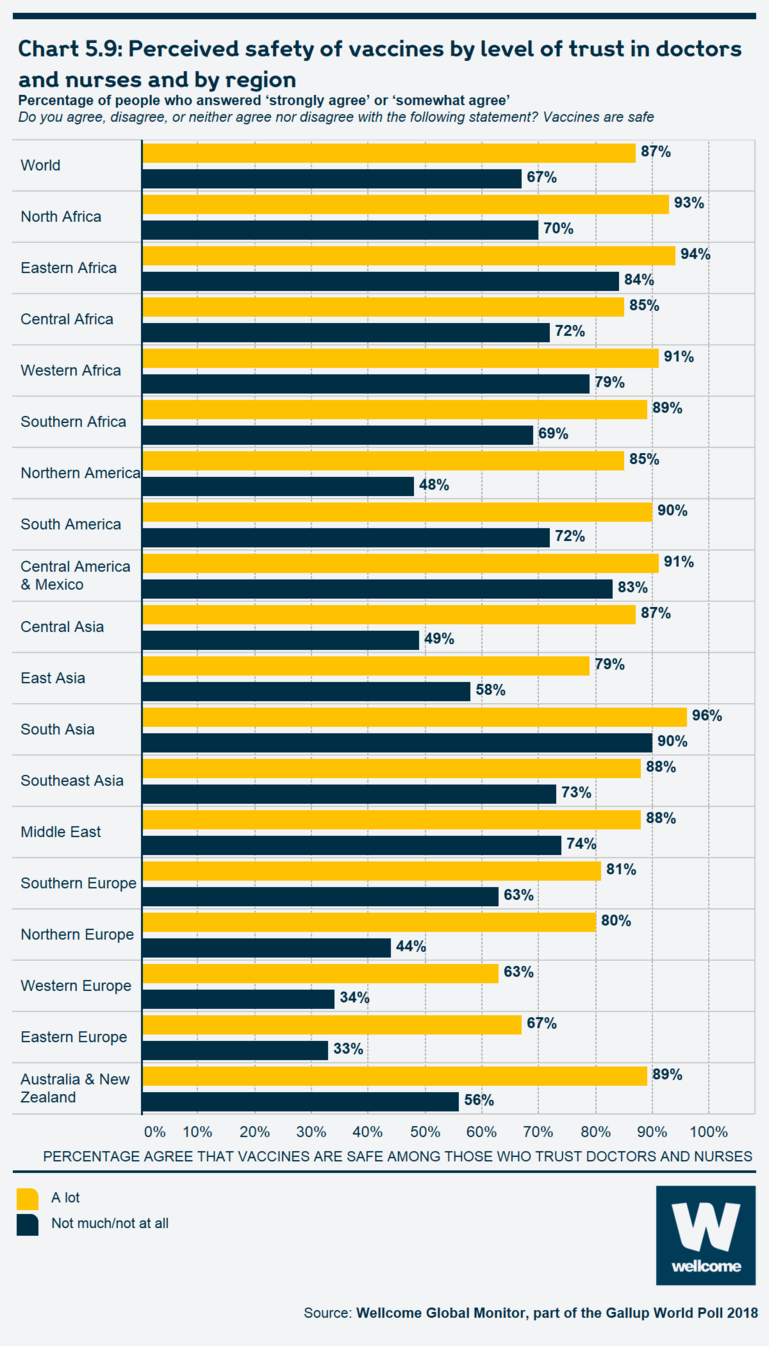
See the interactive version of this chart.
Conclusion
Wellcome Global Monitor shows that confidence in vaccines is generally very high across the world, particularly in lower-income countries. People in high-income countries have less confidence – most people in these regions think vaccines are effective at preventing infectious diseases, but a significant minority (50% in Eastern Europe) have concerns over safety. And in some of these regions, greater scientific knowledge or levels of education is actually associated with less confidence in vaccines. This suggests that putting out more scientific information, or trying to educate more people, will not be enough to change minds on this issue.
In France, one-third of people do not agree that vaccines are safe, but only 19% disagree that they are effective. Just 10% disagree that it is important for children to be vaccinated – although if 10% of people remain unvaccinated against measles, for example, that can be enough to allow the infection to spread and cause dangerous outbreaks.
People with more trust in scientists, doctors and nurses tend to be more likely to agree that vaccines are safe. Conversely, those who have sought information about science, medicine or health recently appear to be less likely to agree. There is no evidence of what information people were seeking, but is there something about people who actively seek science and health information, or the information they find, that means they are more likely to be sceptical about vaccines?
Globally, more than 90% of parents say their children have been vaccinated, and even in countries like France, it would appear that many people who doubt the safety or effectiveness of vaccines still agree to having their children vaccinated. However, recent outbreaks of measles in the US, Brazil and India suggest that we cannot take herd immunity for granted – understanding trends in people’s attitudes to vaccines will be critical to maintaining public health in the years ahead.
If any interactive charts are slow to load, try later or contact our team at wgm@wellcome.org.
Endnotes
- Wellcome. Vaccines: A world equipped to combat infectious disease. https://wellcome.org/what-we-do/our-work/vaccines [accessed 13 May 2019];
- World Health Organization. 10 Facts on Immunization. 2018 March. https://www.who.int/features/factfiles/immunization/en/ [accessed 13 May 2019].
- World Health Organization. Immunization, Vaccines and Biologicals: Addressing Vaccine Hesitancy. 2018 12 September. https://www.who.int/immunization/programmes_systems/vaccine_hesitancy/en/ [accessed 13 May 2019].
- Stern A, Markel H. The History of Vaccines and Immunization: Familiar Patterns, New Challenges. Health Affairs 2005;24(3):611–21.
- Larson HJ, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016;12:295–301.
- Barrows M, et al. Parental Vaccine Hesitancy: Clinical Implications for Pediatric Providers, Journal of Pediatric Health Care 2015:29(4):385–94.
- Onnela JP, et al. Polio vaccine hesitancy in the networks and neighborhoods of Malegaon, India. Social Science & Medicine 2016;153:99–106.
- Diekema DS. Improving Childhood Vaccination Rates. The New England Journal of Medicine 2012;391–3.
- World Health Organization. Immunization, Vaccines and Biologicals: Addressing Vaccine Hesitancy. 2018 12 September. https://www.who.int/immunization/programmes_systems/vaccine_hesitancy/en/ [accessed 13 May 2019].
- World Health Organization. Ten threats to global health in 2019. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 [accessed 13 May 2019].
- Larson J, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016;12:295–301, and at: https://www.vaccineconfidence.org/research/the-state-of-vaccine-confiden...
- The actual questions and response options were broken down into ‘branching’ sub-sections so that they formed a lower response burden on the respondents across different education levels. Please see the full questionnaire in Appendix B: Questionnaire [PDF 2.13MB].
- Fine P, et al. 'Herd immunity': A rough guide. Clinical Infectious Diseases;52(7):911–6. https://academic.oup.com/cid/article/52/7/911/299077 [accessed 14 May 2019].
- Sadarangani M. Herd Immunity: How does it work? Oxford Vaccine Group 2016 26 April. https://www.ovg.ox.ac.uk/news/herd-immunity-how-does-it-work [accessed 14 May 2019].
- Tannous L, et al. A short clinical review of vaccination against measles. JRSM Open 2014;5(4):1–6, April 2014. https://journals.sagepub.com/doi/10.1177/2054270414523408 [accessed 14 May 2019].
- Onnela JP, et al. Polio vaccine hesitancy in the networks and neighborhoods of Malegaon, India. Social Science & Medicine 2016;153:99–106.
- Sadarangani M. Herd Immunity: How does it work? Oxford Vaccine Group 2016 26 April. https://www.ovg.ox.ac.uk/news/herd-immunity-how-does-it-work [accessed 14 May 2019].
- European Centre for Disease Prevention and Control. Influenza vaccination coverage rates in the EU/EEA. 2018. https://ecdc.europa.eu/en/seasonal-influenza/prevention-and-control/vacc... [accessed 14 May 2019].
- Centers for Disease Control and Prevention. Estimates of Influenza Vaccine Coverage among Adults – United States. 2017–18 Flu Season. 2018 25 October. https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates.htm [accessed 14 May 2019];
- UNICEF. ‘Alarming global surge of measles cases a growing threat to children.’ Press release: 28 February, 2019. https://www.unicef.org/press-releases/alarming-global-surge-measles-case... [accessed 14 May 2019].
- Centers for Disease Control and Prevention. Measles: It Isn’t Just a Little Rash [Infographic]. 2018 5 February. https://www.cdc.gov/measles/parent-infographic.html [accessed 14 May 2019].
- UNICEF. ‘Alarming global surge of measles cases a growing threat to children.’ Press release: 28 February, 2019. https://www.unicef.org/press-releases/alarming-global-surge-measles-case... [accessed 14 May 2019].
- World Health Organization. Immunization, Vaccines and Biologicals: Measles and Rubella Surveillance Data. 2019 13. https://www.who.int/ immunization/monitoring_ surveillance/burden/vpd/surveillance_type/active/measles_ monthlydata/en/ [accessed 14 May 2019].
- Larson HJ, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016;12:295–301, and at https://www.vaccineconfidence.org/research/the-state-of-vaccine-confiden... [accessed 14 May 2019].
- There is substantial variation by country in Eastern Europe, with country-level results significantly below the population-weighted regional figure of 50% in the following countries: Ukraine (29%), Belarus (41%), and Bulgaria (44%). The results for the following countries are above the regional aggregate: Czech Republic (69%), Hungary (79%) Poland (81%), Romania (69%) and Slovakia (77%). The weighted regional aggregate is affected by Russia’s large population, where the figure stands at 48%.
- Other research shows similar findings, for example: Larson HJ, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016;12:295–301, and at: https://www.vaccineconfidence.org/research/the-state-of-vaccine-confiden... [accessed 14 May 2019].
- Hackett DW. Liberia reports significant infectious disease outbreaks. Precision Vaccinations 2018 19 June. https://www.precisionvaccinations.com/lassa-fever-acute-flaccid-paralysi... [accessed 14 May 2019].
- Kaufmann J, et al. Vaccine supply chains need to be better funded and strengthened, or lives will be at risk. Health Affairs 2011;30(6):1113–21. https://doi.org/10.1377/hlthaff.2011.0368 [accessed 14 May 2019].
- Boulton M, et al. Socioeconomic factors associated with full childhood vaccination in Bangladesh, 2014. International Journal of Infectious Diseases 2018;69:35–40 and at https://www.sciencedirect.com/science/article/pii/S1201971218300365 [accessed 15 May 2019].
- UN Office for the Coordination of Humanitarian Affairs (OCHA). Bangladesh: Diphtheria Outbreak – 2017–2019. ReliefWeb 2019. https://reliefweb.int/disaster/ep-2017-000177-bgd [accessed 14 May 2019].
- Schwarzinger M, et al. Low Acceptability of A/H1N1 Pandemic Vaccination in French Adult Population: Did Public Health Policy Fuel Public Dissonance? PLOS ONE 2010;5(4):1–9 and at https://doi.org/10.1371/journal.pone.0010199 [accessed 14 May 2019].
- Bruhl D, et al. Extension of French vaccination mandates: From the recommendation of the Steering Committee of the Citizen Consultation on Vaccination to the law. Euro Surveill 2018;23(17).
- Le Monde with AFP. WHO justifies its management of influenza A. Le Monde 2010 26 January. https://www.lemonde.fr/epidemie-grippe-a/article/2010/01/26/l-oms-justif... [accessed 14 May 2019].
- Rey D, et al. (2018). Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Euro Surveill 2018;23(17). https://doi.org/10.2807/1560-7917.ES.2018.23.17.17-00816 [accessed 15 May 2019].
- UNICEF. Alarming global surge of measles cases a growing threat to children. 2019 28 February. https://www.unicef.org/press-releases/alarming-global-surge-measles-case... [accessed 14 May 2019].
- Synovitz R. Are Russian trolls saving measles from extinction? Radio Free Europe/Radio Liberty 2019 13 February. https://www.rferl.org/a/are-russian-trolls-saving-measles-from-extinctio... [accessed 14 May 2019].
- Fine PEM. Herd Immunity: History, Theory, Practice. Epidemiologic Reviews 1993;15(2):265–302. https://doi.org/10.1093/oxfordjournals.epirev.a036121 [accessed 14 May 2019].
- Diseases referred to in the question varied by country according to which types of vaccinations were most common; in some regions, the question referred to 'childhood diseases such as measles, mumps, or rubella'.
- Saitoh A, Okabe N. Progress and challenges for the Japanese immunization program: Beyond the 'vaccine gap'. Vaccine 2018; 36(30):4582–8 https://doi.org/10.1016/j.vaccine.2018.01.092 [accessed 15 May 2019].
- Tanaka Y, et al. History repeats itself in Japan: Failure to learn from rubella epidemic leads to failure to provide the HPV vaccine. Human Vaccines & Immunotherapeutics 2017;13(8):1859–60. https://doi.org/10.1080/21645515.2017.1327929 [accessed 15 May 2019].
- The Japan Times. Japan's backward vaccination policy. The Japan Times. 2018 26 June. https://www.japantimes.co.jp/opinion/2018/06/26/commentary/japan-comment... [accessed 14 May 2019].
- Sandhofer MJ, Robak O, Frank H, Kulnig J. Vaccine hesitancy in Austria: A cross-sectional survey. Wien Klin Wochenschr 2017; 129(1–2):59-64 https://doi.org/10.1007/s00508-016-1062-1 [accessed 15 May 2019].
- A similar relationship holds for the other two questions about vaccines, though not as noticeable as this question. This is why this item is being singled out in this section.
