How we can make better use of antibiotics – a research roadmap
Antibiotics have been saving millions of lives for decades, but we’ve now reached a point where we need to save antibiotics. A global research roadmap funded by Wellcome shows how.

lakshmiprasad S / iStock
The rise of drug-resistant infections – which are killing hundreds of thousands of people every year – is now one of the biggest threats to global health.
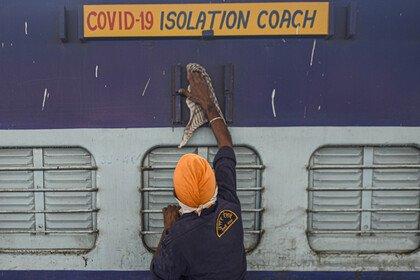
It has been fuelled by decades of inappropriate use of antibiotics in humans. The Covid-19 pandemic might have contributed to this too, as early reports suggest.
While we need to bring new antibiotics to market, we also need to preserve and sustain the efficacy and longevity of existing ones and protect the effectiveness of future drugs.
Leaders at the recent G7 meeting have also acknowledged this as a priority for global health. So how do we make better use of our antibiotics?
Optimising the use of antibiotics is a complex issue
Socio-cultural contexts and shifting population and individual characteristics play a big part in how antibiotics are used.
In low- and middle-income countries, where the largest health and economic burdens from drug-resistant infections are disproportionately felt, there are other factors too: lack of guidelines, limited therapeutic choices, a lack of prescribers and disruption of supply chains.
So measures to improve antibiotic use developed for one country may not necessarily work in another. Similarly, developing a technology to improve antibiotic use does not mean it will automatically be adopted.
To make change happen, we have to recognise and address the wider factors that influence antibiotic use, and overcome the challenges facing research implementation in this area.
This is why we commissioned a global research roadmap for optimising the use of antimicrobials in humans. The roadmap is for researchers to consider when developing new research proposals, and for research funders and policy makers who can influence future funding opportunities and the implementation of research.
To find out more about this research, read the full report in The Lancet: Optimising antimicrobial use in humans – review of current evidence and an interdisciplinary consensus on key priorities for research. Or you can read the highlights below.
A research roadmap to optimise the use of antimicrobials in humans
To develop the roadmap, a team led by experts at Imperial College London reviewed current evidence and engaged with a diverse group of international stakeholders.
They identified research priorities across four broad themes:
- policy and strategic planning
- medicines management and prescribing systems
- technology to optimise prescribing
- context, culture and behaviours.
Alongside these themes, three systems-level issues, which are cross-cutting, need to be considered:
- the need to capture the economic impact of drug-resistant infections and the required solutions
- the impact of external shocks on the problem of drug-resistant infections (for example, the Covid-19 pandemic) and the need to sustain societal focus and research
- the requirement for equitable capacity building and knowledge mobilisation.
So, what do we need to see from future research streams to optimise antimicrobial use in humans?
- make better use of existing hospital and community data for optimal prescribing
- improve integration and engagement between sectors and stakeholders to highlight the need for action
- develop the building blocks of responsive health systems
- address supply and prescribing systems’ needs to improve access to antimicrobials
- identify culturally and contextually appropriate interventions to help ease local uptake
- develop assessment frameworks to help ensure economic and equitable distribution of technologies
- develop sustainable public engagement mechanisms for people most at risk
- ensure everyone has access to optimally prescribed antimicrobials regardless of socioeconomic and cultural status.
The roadmap maps research priorities across a ten-year timeline. Have a look at the research roadmap in a PDF format [PDF 555KB], or explore the graphics below.
Graphics: the research roadmap to optimise the use of antimicrobials in humans
Click images to open gallery
While priorities at national levels may differ, within two years countries should have a detailed understanding of the challenges they face and begin developing appropriate policies and interventions. Within five years they should be implementing them and refining their approach. Finally, by ten years they should be moving to a sustainable model of research and evaluation.
What’s next for Wellcome
At Wellcome we are using these findings to underpin and direct our work and the activities we fund. International collaboration and equitable partnerships will be central to our approach.
However, we cannot do this alone. Researchers, funders, policy makers, citizens, civil society, patients, and the public need a sense of ownership and responsibility for not only the challenges, but the solutions to optimising antibiotic use.
And we need dynamic action at national, regional and global levels: to recognise the complexity of the challenge, allocate the technical and financial resources needed, and foster close links between research and policy.
We have the roadmap – now we need to work together to implement it.
If you would like to learn more about our approach to optimising antibiotic use, we hope to share more soon, in the meantime get in touch at drugresistantinfections@wellcome.org.
Graphics: why optimising the use of antimicrobials is important
Click images to open gallery