When I talk to patients who have Parkinson’s disease in my clinic, the one thing that terrifies them is that they could develop dementia. Their worries are not unfounded.
Studies have found that nearly 50% of people with Parkinson’s disease will develop dementia within ten years of diagnosis. It's common to think about Parkinson's as a movement disorder. But actually, people with Parkinson's are six times more likely to get dementia than the general population.
The problem is we don’t fully understand why this happens. In fact, at the moment, there are no treatments that change the course of Parkinson's. We've got good treatments that help with the symptoms, but they don't change the ultimate course of the disease. And if patients are beginning to develop dementia, we can't stop that either.
That’s why I’m pursuing my current research.
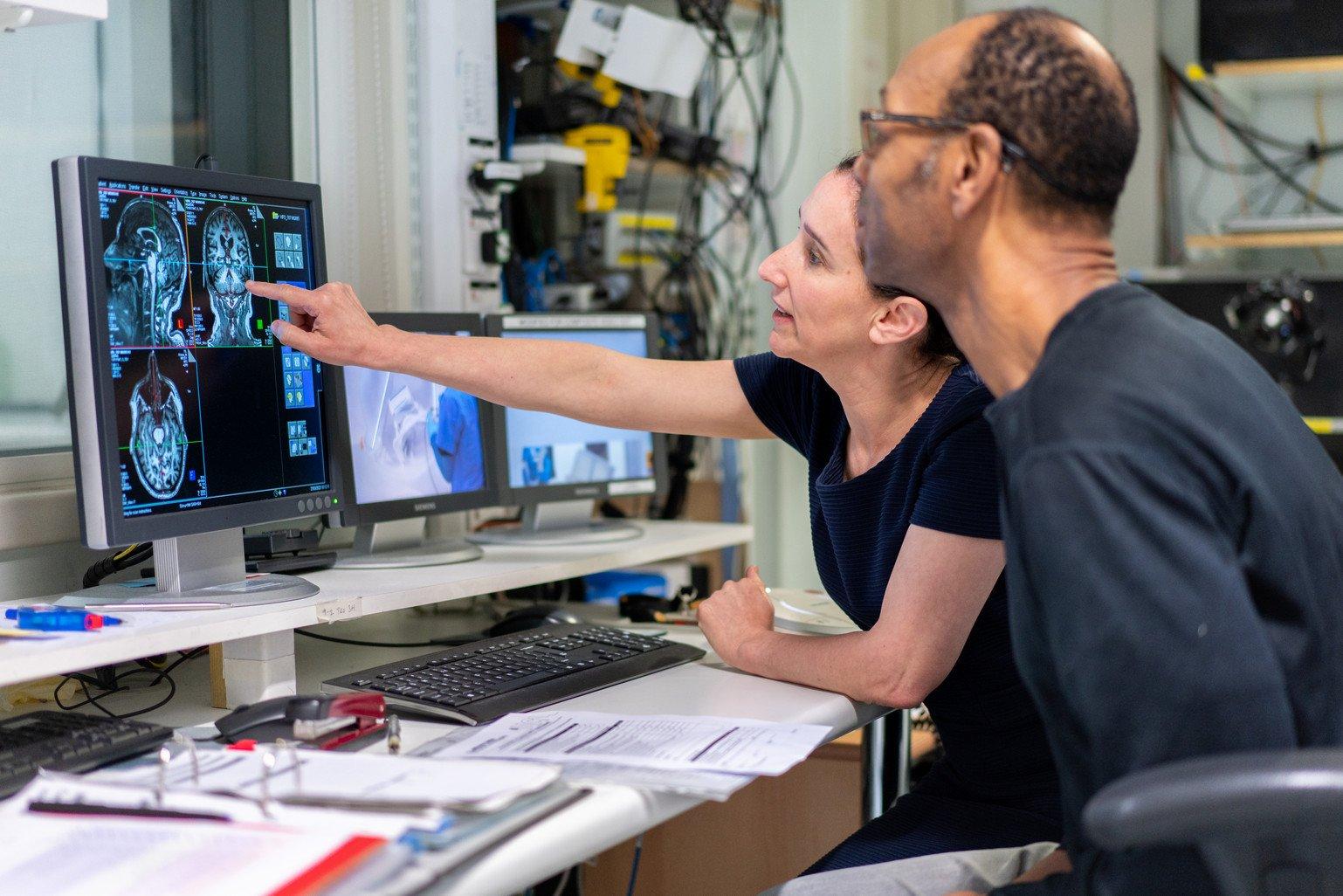
Advanced neuroimaging to understand the brain
To understand the disease, we must first have a better sense of what changes take place in the brains of people living with the condition. We can do this with the help of advanced neuroimaging.
The aim of my research is to bring together advanced neuroimaging with measures of protein accumulation, or the build-up of proteins in the brain.
The advanced imaging that I'm carrying out uses measures of brain connections and measures sensitive to brain iron. I'm also scanning using high-field MRI (or magnetic resonance imaging, used to form pictures of the body). This provides me with greater spatial resolution of the brain.
I’m also using other approaches so that we can measure protein accumulation in the brain. To do this, I'm collecting blood and cerebrospinal fluid. I'm collaborating with chemists so that we can accurately measure the levels of proteins in people's blood and in their cerebrospinal fluid. Alongside this, I’m using PET imaging (or positron emission tomography, which produces 3D images of the inside of the body), which can directly measure particular proteins that build up in the brain.
Ultimately, my aim is to be able to identify which particular combination of proteins is building up in the brain for each patient, so we can understand that person’s disease better.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
At the moment, there are no treatments that change the course of Parkinson's disease. We've got good treatments that help with the symptoms, but they don't change the ultimate course. And if patients are beginning to develop dementia we can't stop that.
I'm Dr Rimona Weil, I'm a neurologist, a neuroscientist at UCL, working on Parkinson's disease dementia. My vision is to understand how dementia happens in Parkinson's disease.
People think about Parkinson's as a movement disorder. But actually, people with Parkinson's are six times more likely to get dementia than the general population.
And if we really want to get to understand that fully, we need to link together changes that happen in the brain in people living with the condition, which we can do using advanced neuroimaging. And then what we want to is link that with the proteins that build up in the brain. So we need to obtain measures of protein accumulation from the same patients at the same time.
So that one day we can have a patient who comes to my clinic and I'm worried that they're developing Parkinson's disease dementia, and I'd be able to say to that specific person, well you have this particular pattern of changes.
So this new treatment that's been developed would be right for you. Whereas another patient might have a different pattern of changes and then we would be targeting different treatments.
When I was working as a clinical neurologist, I noticed that people with Parkinson's disease not only developed dementia but actually seem to have trouble, particularly with visual tasks. And that became a much bigger project. And we found that over time, patients with Parkinson's disease who had visual problems really did develop cognitive change, and we're now using that in this project to stratify patients so that we can then compare patients with Parkinson's who don't yet have dementia but do have visual problems. So that we can then look at the differences in their brain to try to understand the basis of these really early changes.
If we take a person with Parkinson's disease and we do a conventional hospital type MRI scan, we don't really see any changes. And in fact most of my patients in clinic have been told that their MRI scan is normal.
But what I'm able to do with this project is use advanced neuroimaging, which starts to provide new information, actually about the structures of the tissues. And that's actually allowing us to quantify changes, and then I'll be able to link that also to the protein changes. And that's what's really new about this project – to be able to really look at the changes in the tissue composition in patients with Parkinson's disease.
So having a Discovery Award has really allowed me to think big and broad about the questions that I'm trying to address. So as well as doing advanced imaging, actually using two different types of MRI scanners, I'm also doing PET imaging measures of plasma, also measures of cerebrospinal fluid and also magnetoencephalography.
So I'm getting, really, information across the range of different modalities that are all looking to address the same question.
But it's through the Discovery Award that I can really be quite ambitious about the questions that I'm asking.
So it was the broadness, the length of time, and also the flexibility of the funding that I could apply it to a question that is clinically important, but also of importance to neuroscience as well.
The right treatments for patients
As new treatments are being developed, knowing which proteins are building up – and understanding the changes in the brain early on before the disease sets in – will help us target the right treatments for the right people.
The work that I'm doing will have wider relevance for other causes of neurodegeneration. My work is focused on Parkinson's dementia, but my findings will have applications for other dementias and potentially for other neurological conditions.
I'm doing this research because, ultimately, I want to be able to slow the progression of Parkinson's dementia by targeting the right treatments to individual patients. I also want to bring some of the advanced imaging measures we are using in my research into clinical pipelines, so that we can monitor disease progression in patients who are seen in the clinic.
My aim is that one day, when I’m seeing a patient in my clinic, and I'm worried they're developing Parkinson's dementia, that I'd be able to say to that specific person: 'Well, you have this particular pattern of changes. So this new treatment that's been developed would be right for you.'
Thinking big
As well as doing advanced imaging – using two different MRI scanners – I'm also using PET imaging, measures of proteins in the plasma and cerebrospinal fluid and also MEG (magnetoencephalography, which measures or maps brain activity through magnetic fields generated in the brain). Together, these different modalities will provide information across a range of spatial scales. I will do this in people living with the condition to address the same question: how does dementia happen in Parkinson’s?
All this is possible because of Wellcome’s Discovery Research Career Development Awards. The award has allowed me to be ambitious about the questions that I'm asking and think much more broadly.
Wellcome funding allows me quite a lot of flexibility and that's what's really attractive about this award. It allowed me to apply for it as a clinician and as a scientist. It was flexible in terms of time – this is an eight-year project – and it's also flexible in terms of the questions that I'm asking.
Through discovery science, I am able to work on this really important research question that addresses the real-world problem of Parkinson's dementia. Hopefully, this work can ultimately help ease some of that worry among patients by helping to target the right treatments to the right patients at an early stage in their disease progression.
Wellcome supports bold and creative discovery research that has the potential to improve human life, health and wellbeing.
We have three recurring funding awards:
Explore our one-off funding awards: