
The first Covid-19 vaccine may not be the magic bullet that returns life to 'normal'
As we'll soon start to see the results of the first vaccines coming through late-stage clinical trials, Jeremy Farrar explains why we should be cautiously optimistic.
At the end of any summer, we brace ourselves – for back to school, returning to work and even for Christmas plans. But this year, the reality bump is like no other.
The long road ahead
As the Covid-19 pandemic continues to reverberate globally, there is no doubt that we must be ready to face a long road ahead, certainly beyond the end of this year. The fact that a vaccine, alongside effective treatments, is our only true exit strategy remains unchanged. The speed and scale of vaccine development have been remarkable but it’s important to avoid false hope.
I am optimistic that we will soon see results from the first vaccines coming through late-stage clinical trials. However, we must temper this optimism, this talk of the perfect vaccine 'just around the corner' or the idea that it will be a complete and immediate solution.
Over the summer, the UK vaccine taskforce has done an impressive job of securing access to a broad portfolio of potential Covid-19 vaccines. But I worry that, beyond the taskforce, too much hype is being applied to the first vaccines, and in some countries too much focus on a political agenda and domestic provision. There should be no place for notions of vaccine nationalism, with nations posturing that 'their' vaccine will cross the finish line first and be fully deployed by Christmas or for a political moment.
The first generation of Covid-19 vaccines
The 'first' vaccine, or even the first generation of vaccines, will most likely not be perfect; we need to be pragmatic and transparent on that front. The reality is that with these vaccines, we will be taking small steps to return to a sense of normality.
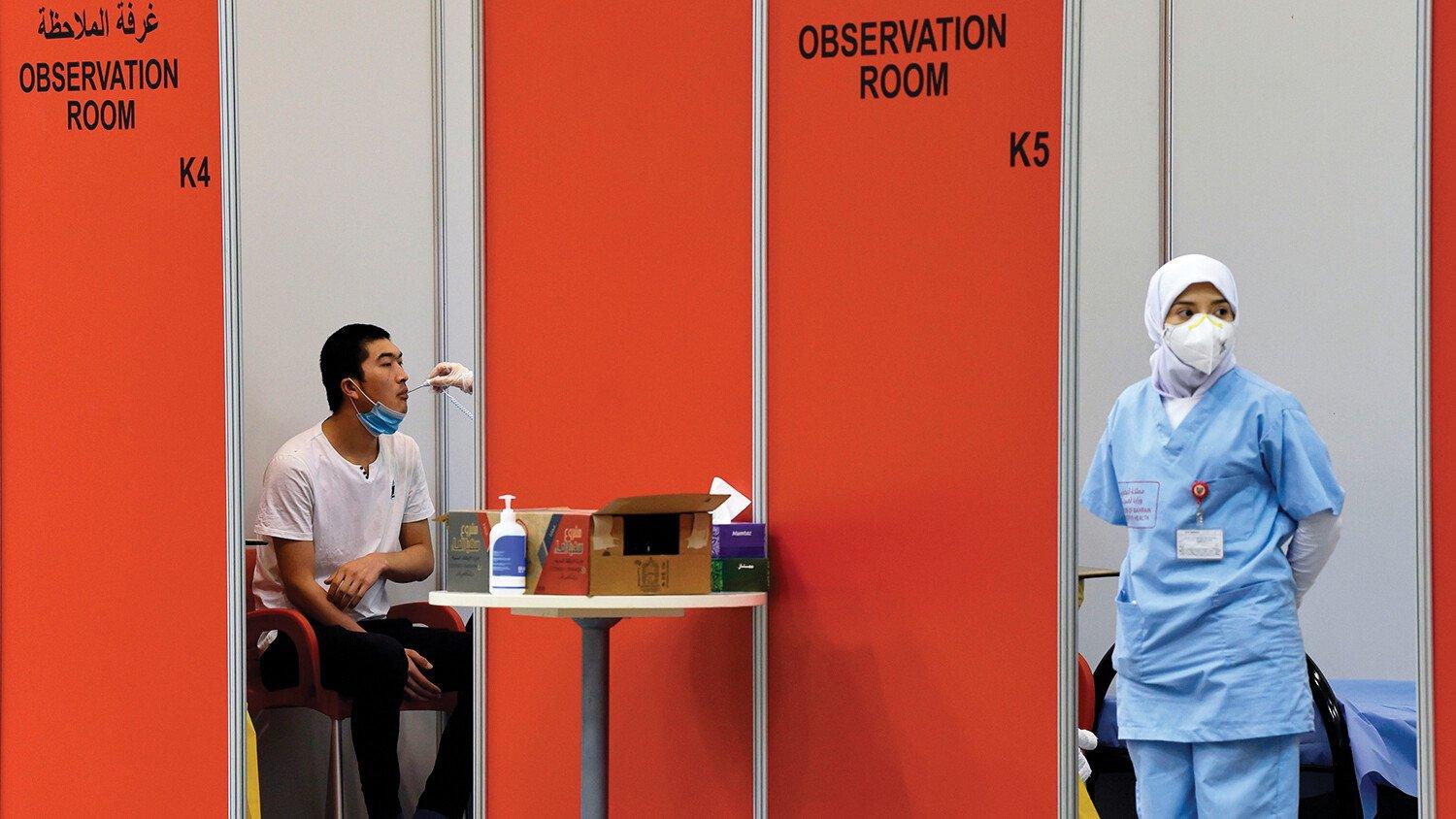
Plenty is attached to the word vaccine. When we hear it, we think of one of the greatest advances in human health, one that eliminates smallpox and saves millions every year from polio and tetanus, from HPV and the flu. However, the first generation of Covid-19 vaccines will probably be only partially effective. They might not be completely effective in all ages or appropriate in all health systems. It is very possible that they might provide immunity only for a limited period, even as short as 12 to 18 months. This might not be what we are used to from a vaccine, but there is no doubt that the first effective vaccines, even imperfect ones, can have a major impact and be a precious commodity.
Urgency must not be misunderstood; accelerating vaccine development must not mean compromising safety. Transparent, rigorous assessment by independent regulatory bodies without political interference is non-negotiable. Trust is our most important tool in public health and we must do everything we can to avoid putting that in doubt. It cannot be bought on short-term promises. Already, there are worrying signs of diminishing trust in potential Covid-19 vaccines. Polls suggest that in countries with some of the highest global case numbers, such as the United States, there could be low uptake of any Covid-19 vaccine, no matter how effective. This must not become a polarised political issue, public health is too important.
Most importantly, fair access to any vaccine must be addressed. No matter where the first vaccines originate, they must initially reach priority groups worldwide, particularly frontline healthcare workers and the most vulnerable. Global cooperation is key to advancing these vaccines and restarting the global economy. If large parts of the world remain shut down because of the selfish hoarding of initial supplies by richer nations, we all suffer for it.
It is not, however, enough to simply promise support for fair, global allocation. More nations must act with urgency and buy into a collective and pooled approach to vaccine access, all governments being clear they will buy doses only for the most at risk in their populations.
Ensuring equal access to affordable vaccines
The United States not joining the vital COVID-19 Vaccines Global Access Facility (COVAX), which aims to ensure equal access to affordable vaccines, is disappointing. It is more imperative than ever that those in stronger positions, with considerable resources, lead by example in fair allocation.
The UK has manoeuvred itself into such a leading position. It has options on a 340 million dose stockpile, the highest access per capita of any country. Yet only 20%-30% of the UK population will require access to a vaccine in the first few months. The UK’s position could be even stronger through firm commitments to pooling surplus doses through COVAX. The European Commission has also shown important leadership and has committed €400 million, but it too is in a strong position to do more. Such enlightened global leadership is badly needed at this time of crisis.
As we move through autumn and winter, we will see an increase in community transmission. Without urgent action to stop the current increased community transmission among young adults leading onto transmission in hospitals and in social care, and thereby severe illness and deaths in vulnerable people, we will be facing a chaotic stop-start winter for schools and businesses.
We have to do everything possible to avoid this. The first vaccine may not be a magic bullet that sends us back to normal in a matter of months. However, by using doses wisely on the people who most need them – and doing this alongside truthful, considered public health messaging that does not deal in false expectations – we will be in a strong position to avoid a repeat of early 2020.
This article was first published in The Observer on 6 September 2020.


