Episode 7: How can volunteering to be infected save lives?
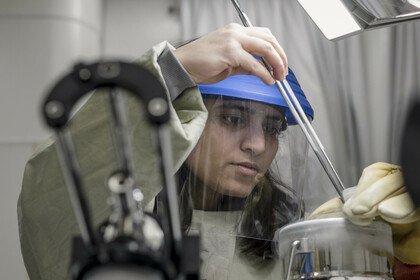
Human infection studies are a quick and effective way to gather data to see whether or not a vaccine is working. Alisha speaks with Dr Dingase Dula to learn more about the impact of infection studies in combating infectious disease.
Listen to this episode
Dingase Dula 00:02
We want those crystal-clear answers that we can give to policymakers so that they can maximise the potential of this vaccine. Because it works, yes, but it could work better if we just study it closely in our population.
Alisha Wainwright 00:18
Welcome to When Science Finds a Way, a podcast about the science changing the world.
I’m Alisha Wainwright, and on this series, I’m meeting with scientists and researchers who are actually making a difference, as well as the people who have inspired and contributed to their work.
Now, when I first heard the phrase, “human infection studies”, I was intrigued. There are some other names for this kind of research, like human infection trials, or human challenge studies. But the concept is the same – you give a volunteer a vaccine or some other intervention, and then infect them in a controlled environment so you can observe how effective your intervention is.
Globally, infectious disease is a huge health issue. That’s especially true in Africa, where about half of all deaths are caused by infectious disease. Yeah – that’s huge.
So, to get more insight into this critically important research, I spoke with Doctor Dingase Dula. She recently led a human infection study in Malawi, as part of her role as lead physician with the Malawi-Liverpool Wellcome Trust Research Programme.
That’s a partnership between researchers based in Liverpool in the UK, and Malawi. You’ll hear Dingase call it MLW for short.
Human infection studies are done all over the world, and Dingase explained why they’re so important in the fight against infectious disease. She emphasised how these studies are strictly controlled for safety, and also connected us to some volunteers who took part, and were happy to share their experience.
Becky Mkandawire 02:07
They taught us that, if anything, you can come to the clinic, and they give us the numbers of the doctors that we could contact. So I knew that I was very safe about it. So I knew taking the risk was just perfect for me.
Alisha Wainwright 02:19
Dingase’s human infection study was a replica of one originally done in Liverpool. Now, that research has been conducted in Malawi – with local scientists and local volunteers. This is kind of a new thing in Malawi – and she told me about the benefits of this locally-led research.
Dingase Dula 02:38
So they've really empowered a lot of Malawian scientists to really lead this work. Yeah, moving forward, because this is work that has the potential to have a lot of public health benefits, as well as clinical benefit. And Malawians are at the forefront of doing these studies.
Alisha Wainwright 02:54
This conversation gave me some real insight into the range of issues that come up in developing and researching a vaccine. For example, uptake of Covid vaccines in Malawi is relatively low compared to many other countries. Why is that? Could Malawi-led research change these attitudes?
We talked about all this, and more. But to start off with, I asked Doctor Dingase Dula to give us some context – exactly how does a human infection study work?
Dingase Dula 03:34
So a human infection trial is a kind of study where you get a healthy volunteer, and you introduce a pathogen, so it can be bacteria, or a virus, to this healthy individual, in order to understand the interaction between the individual and this pathogen. This kind of trial is done in a very well controlled setting. So you know, the dose of organism you're giving, so you characterise it in the lab, you know exactly what you're giving, you know how to stop that infection, or to stop progression of that infection. So you have to test the organism to see what kind of drugs it responds to. The volunteer has to be monitored very closely, by a very well experienced team of doctors and nurses, most of the times after - they have to quarantine for a defined period.
Alisha Wainwright 04:32
Or else you're gonna find yourself with some extra participants…
Dingase Dula 04:36
Yeah, yeah. So you quarantine them, and then you need to have a way to measure the bacteria, or the virus, or whatever pathogen that you've introduce. You need to find a way to measure, such that, when they are leaving your trial, you make sure that they are pathogen free. If they haven't cleared that bacteria or virus, you give them a medication so that they go home, they're fine.
Alisha Wainwright 05:00
So what are the advantages of these kinds of trials, why do them?
Dingase Dula 05:04
These trials are actually more favourable, because you, because you're controlling everything, right? You're not waiting for, for example, disease to happen. You’re even controlling the outcome, you decide when to terminate the infection, and so on. You tend to get your answers a bit quick, than in other types of trials, right?
So I'll give an example. So if I want to study, maybe streptococcus pneumonia, that's the type of bacteria that commonly causes pneumonia, sepsis, and so forth. You can introduce the pathogen today. The follow up period will be maybe another two to three weeks. After two to three weeks you collect samples. And depending on the number of volunteers you have, in a couple of months, you can have the outcome that you're looking for. You can have your answers to your research. So that's actually one of the advantages of a trial, because everything is so well controlled. You get results a bit faster. And you don’t need to get, for example, hundreds of thousands of participants. With tens, and even hundreds of participants, you can have substantial answers.
So for example, you have, if you have three promising vaccine candidates, but you're not sure which one to invest a lot of resources in, or which one to test in a lot of people - human infection trials are important in this process. So it's called down-selection of vaccines. So you have, for example, three potential candidates - vaccine candidates - and you're like, okay, which one should I move forward? Yeah, so you can conduct a human infection trial. So in a couple of months, or maybe in a year, you have a sense of, okay, I think this is the most promising candidate, then I can move on to invest a lot of resources to test it in more people, in a larger trial. This is what human infection trials are used for. So they are used to select the most promising vaccine candidates, or the most promising treatments, to test them on a larger scale, so that you don't waste time and resources on something that will not work,
Alisha Wainwright 07:19
Mm-hm, or not work as efficiently as maybe another candidate?
Dingase Dula 07:22
Exactly.
Alisha Wainwright 07:25
I mean, I'm just gonna come out and say it - human infection trials, they sound scary, you know, why do we do this kind of research?
Dingase Dula 07:32
It does sound scary. And I think, even to myself as a doctor, it's something that I had to really understand, to take time and understand, you know, the science, and compare it to other kinds of trials. But human infection trials are actually some of the safest trials. Because everything is just so well controlled, yeah? You know exactly what you're giving. You are in control of when you terminate the infection, yeah? Because you don't give a bug that, for example, is not responsive to medication. It has to be done under such strict conditions, by people who have the best skills to ensure that. So safety is of paramount importance.
So human infection trials control for a small number of people, relatively, they are safer, fewer serious illnesses, no records of death. So in Africa, there are several sites where human infection trials are being done for several pathogens. In the UK, in the US, the data is very consistent that these trials are very safe. I think it's because there's just too much precaution to ensure that people don't get seriously ill or die from participating in this trial.
Alisha Wainwright 08:56
Okay, well, we're going to hear from two participants in your human infection trial, Becky and Stonard. We asked them about why they decided to take part and why others were reluctant.
Becky Mkandawire 09:11
After they came here, they told us the information, and then they gave us an option that we should go home and think about it. And when we think about it, and then if we want to join it, then we should give them a call. So when I went home, I explained it to my aunt, actually she's a doctor at Baylor College of Medicine. So I asked her if the study's okay, are there any challenges that we're going to meet? Because a lot of people were talking about a lot of things - bad things, negative things, so that maybe I shouldn’t join: ahh, don't go there, actually they're going to give you the bacteria, they will give you viruses, so many things. So I wanted to verify with her. So she told me that it's okay. Most of the time, she conducts so many studies, so many surveys with the Malawi Liverpool Trust, you can go ahead, there's nothing wrong with it. So after hearing from her, it's when I called back the Malawi Liverpool Trust guys, and told them I was interested, that I wanted to join.
Stonard Mwale 10:06
Before taking part into the study, before you are given the vaccine or not, they have to test you if you're HIV positive or not. Generally people are afraid of being tested, because maybe some of the people they have never been tested in their lives in terms of HIV and AIDS. That's why people - they’re very afraid.
So a lot of things were being said about the vaccines. But I think I was confident enough because I knew what I was doing. Most of the people, when I tried to tell them about what I heard, and then what I read through the forms, the leaflets, I think they were quite impressed. I think this is a new thing to do, yeah, so…
Alisha Wainwright 10:53
We heard just then from Becky and Stonard about false information and rumours that were spread about the study. How does your team address that?
Dingase Dula 11:02
Before anybody signs anything there’s a visit that we call an information visit. So we have participants who just pass by the clinic, just to hear about the study. Yeah, so we give them information, verbally - they have a chance to ask questions, we show them all the equipment that we work with, we show them the place that they're going to quarantine in, we show them pretty much everything. So we are not shy, even if we go on radio or on TV, or on, we go to a school in the community - we are not shy about the process that we're going to - so we don't sugar-coat the fact that you're going to get live bacteria. We're very upfront with that to say, this is a human challenge trial. And this bacteria is live bacteria, I mean, we will do everything that we can to make sure you don't get sick. But this is live bacteria, there's a real risk here, that you could get sick. So you really need to think about it, to make sure that you, you really want to join this. And so we are very forthcoming with the information. So I think people know, we're very transparent with our processes. We don't hide anything. So the people that are not willing, or maybe are lukewarm, they don't - those people don't come anyway.
Alisha Wainwright 12:16
But they don't come, but they, but they - now they know. They, like, learn a little bit more. And then if someone down the road is maybe asking them about their experience, it's not a rumour that they're, they're translating, it's something that they learned directly from you. So there is a benefit of just general education.
Dingase Dula 12:32
Exactly. So education is very, very important. We then did a study to even find out from the participants that came, right? We went ahead and asked them what motivated them to come to join the study. It was from hearing about the study from someone who had been in the study. These people, they went on to tell their friends about their actual experience - their lived experience of being in the study. It was like snowballing, yeah? It was just a chain hearing from people who had been in the study. And that is the main recruitment strategy that we used.
Alisha Wainwright 13:08
So, just quickly, can you tell us more about the specific vaccine you've been trialling, and what does it protect against, and who is it for?
Dingase Dula 13:15
So since April 2021, we've been closely studying a licenced vaccine here in Malawi. So this vaccine is called Prevenar, or pneumococcal conjugate vaccine 13. So it's a 13-valent vaccine, which protects against streptococcus pneumonia. So this is a bacteria that causes a lot of disease and death in children - from pneumonia, meningitis and sepsis. But what we noted is that, despite widespread uptake of this vaccine, so all kid, all under-five kids get this vaccine, but we still see a lot of kids getting sick from this same bacteria. So they, we wanted to see why is this vaccine not working as well? Why are kids still getting sick? So because we can't conduct human infection trials in children, we got healthy adult volunteers, and we gave them the vaccine. So we had two groups, one group received the vaccine, and another didn't receive vaccine, but they, we didn't know which group received what, yeah?
Alisha Wainwright 14:26
So that's a double-blind study?
Dingase Dula 14:28
That's a double-blind study. And then, we then inoculated these adults with this bacteria - streptococcus pneumonia. And then when compared carriage. So we, in this particular study we did not study disease, we studied carriage - because carriage is a state where you carry the bacteria in your nose, and you have to carry the bacteria for you to get sick as a result. So then we measured the rates of carriage - we compared the rates of pneumococcal carriage in the nose in the two groups, yeah? So we introduced the streptococcus pneumonia bacteria, it's diluted in - like a liquid. We know the dose we're giving, we introduce it in the nose. And we - the volunteers stay in quarantine for three days. And then we do washes, so we wash the nose, and then we go and culture that liquid in the lab to see who continues to carry, and who clears the bacteria immediately.
Alisha Wainwright 15:26
Let's hear again, from our participants, Becky and Stonard, about their experiences and taking part in the trial.
Becky Mkandawire 15:37
But they taught us that, if anything, you can come to the clinic, and they gave us the numbers of the doctors that we could contact. And most of the time, they were still checking up on us. So I knew that I was very safe about it. So I knew taking the risk was just perfect for me. After being given the bacteria, we were being sent to go to the hotel, where we would spend like three nights there. The food was nice. And then the hospitality was good. And we were being checked on every morning. The matron would come and check to us. So I felt it was very good - that was the first part of my life that I enjoyed [laughs].
They told us that after the study, they were going to tell us if we were being given the bacteria, or if we were given the water. So after the study, it's when they told us that actually I was given the bacteria, and I had some bacteria, so I was being called to come to the clinic to give me medication. But after I was being given medication, everything was okay. It just had, I just had a slight headache, and some flu and cough. But it didn't take long, after the medication there was still checking up on me. So everything was okay. I couldn't complain anymore.
Stonard Mwale 16:49
I always wanted to take part in the study. What they're doing, you see, the vaccine - that will help children. So I thought, I'll be, I'll be taking part and if that meansthe vaccine will be approved. I'll be proud of myself. Because I’ll say, you know, I think at one point of time, I was one of the participants, and then if the vaccine has been approved, that means I played a greater, a greater role on that. So that kind of thinking is what makes me feel proud of taking part.
Becky Mkandawire 17:25
If a friend came to me, and asked me to take part in the study, I would say yes, because at the end of the study, a lot of people will be helped - mainly our kids. So I think the study is a good thing that happened here in Malawi.
Alisha Wainwright 17:47
It sounds like they had a really positive experience. I mean, the food was good, the hotel was good. But putting their experiences aside, what were the findings of your study?
Dingase Dula 18:01
So we found in that study is that the vaccine does work. So the people that received the vaccine, most of them did not carry. So the - to put that in numbers, so the vaccine protects - has 62% protection, 62% in our population. So a perfect vaccine would have 100% protection. That - such a vaccine does not exist, yeah? The best vaccines will confer maybe 78, close to 80% protection. So here in Malawi, the protection of this vaccine, in our study, we found 62%. So this number is still lower than, for example, in settings like the US or the UK. Similar studies that have been done there,the figure is usually 78 or more. So the vaccine doesn't work as well here, which we kind of already knew. So now what we're doing is to try to find out why - why is it that it's not working as well here in Malawi?
Alisha Wainwright 19:00
Okay, so the same vaccine is less effective in Malawi than it is in, say, the US or the UK. And we’ll get into some of the ramifications that has for the research a bit later. But first I wanted to zoom out and just get some context – because, in researching for this interview, I found this stat that only 25% of the Malawi population has received a dose of the covid vaccine - I’d like to ask, in the population there, what is the attitude towards vaccines in general?
Dingase Dula 19:35
So the general population, people view vaccines as something that is supposed to protect children. Because, so we can only as a country, we are only able to vaccinate children. If you go to somewhere like the US or the UK, they're able to vaccinate a lot more vulnerable populations. So for example, people with chronic lung issues, or the elderly, they're able to get jabs, right? But in Malawi, so vaccination is viewed as something that's for children and maybe pregnant women at - for certain few vaccines. For example, I'll give an example of the typhoid conjugate vaccine. It was just trialled here in Malawi. Over 28,000 kids were vaccinated, and, you know, people think - oh, typhoid - typhoid is a disease that happens in children. And children, if they can get a vaccine that prevents, protects children against typhoid, definitely, we'll be happy to have that. The story with the Covid vaccine was completely different. So, people did not want to hear anything about that vaccine, because the concept of you know, first of all, they were like,okay, this disease just came - in a couple of months, we have this vaccine. What? where does this vaccine come from?
Alisha Wainwright 20:47
Is lots of scepticism.
Dingase Dula
You know, there's a lot of scepticism when it comes to vaccines for adults, because it's not something that we really see adults getting vaccinated.
Alisha Wainwright 20:59
Why do you think Malawians feel that way about vaccines?
Dingase Dula 21:03
Maybe, in simple terms, I'd say we don't have the money to give vaccines to adults, you know? We rely on other interventions.
Alisha Wainwright 21:11
So it's almost like, oh, if there's one vaccine, give it to the child, don't give it to me.
Dingase Dula 21:17
Yeah, exactly
Alisha Wainwright 21:18
So it could even almost be like, oh, I don't need it, because it needs to go to the children.
Dingase Dula 21:21
Exactly, it's just the Malawian way for now. To say, okay - if you, if you don't have money to give, if you have limited resources, and all you - if there's a new vaccine, you give it to children, you give it to the under-fives, you know? And that's it after, after five years old, nobody gets vaccines. I think it’s just, it's just the way Malawians perceive vaccines.
So you really have to be careful with your messaging. And, you know, for our trial, we didn't just go straight to doing this kind of trial. We started preparing for this five years ago in 2019. So we just went to the community and just started asking people, do you think this is something that can work in Malawi? What if we introduced a vaccine? Do you think people would do this?
Alisha Wainwright 22:09
Speaking of preparing for your trial – I know that, historically, research like this hasn’t been done within Malawi. So if you need data about a vaccine, it would come from studies done in other countries, like the UK. Why was this the case?
Dingase Dula 22:25
There's this concept that they have to be done in a well resourced setting first, for de-risking, to understand the safety, understand the risks, remove the risks, if possible, or manage the risks, and then transfer it to a lower income setting, who may not be able to cope with maybe unforeseen risks. So far, maybe in the last ten years, that has sort of been the standard, or the way trials are being done, I would say. And it's not necessarily a rule. I think, because African centres that are doing human infection trials, we couldn't just be brave and take, you know, risks that we couldn't manage, yeah? So it hasn't really been a rule as such, or - we can't do this. There's there's nothing preventing us but we do have to be extremely careful in the challenges that we take on.
So now, we sort of weren't mature enough to start off something on our own and take it forward - right - before. But now, regulators even in the UK now they appreciate us - oh, you were able to do this, you you - oh, these are your procedures, okay. I'll give an example for, for the people living with HIV trial, right. That hasn't been done anywhere else in the world. So no one has done an experimental challenge for pneumococcus in people living with HIV. We're going to do it in the, for the first time here. So we will have to mature and really move forward and pioneer some of the things that are of clinical and public health need to us.
Alisha Wainwright 24:05
How important do you think it is for Malawi to take the lead on its own research?
Dingase Dula 24:10
It's, it's really important, because I think, first of all, in the last five years, we now have Malawian scientists and doctors, and social scientists who have these new skills. Before I joined MLW, for example, I was doing other research, but I had never conducted human challenge trials. So they've really empowered a lot of Malawian scientists to really lead this work, moving forward. Because this is work that has the potential to have a lot of public health benefits, and as well as clinical benefit, and Malawians are at the forefront of doing these studies.
You know, speaking about controlled human infection trials, speaking about vaccine trials, I think there's just this sense of trust - to say, okay, perhaps this is something that, you know, is not foreign. So if you, today you were to say, okay, we are trialling this Covid vaccine, or whatever new vaccine, we want to try it for the first time in Malawi, and it's being pioneered by Malawians. People will have that sense of ownership because it's not something that happens in Malawi. Usually, we get a vaccine that is trialled, for example, in the UK. So now it's like we're taking a step back. We're saying no, we're not just receiving vaccines, were actually taking time to test these vaccines in Malawians before they are distributed in the wider population. So it's really important, not just for us working in the trials, but for the general public to say, okay, well you know, it’s ownership, this is actually something that, you know, it's something that we can trust.
Alisha Wainwright 25:48
Hmm, I’m curious, when you’re trying to launch some of the first human infection studies held within Malawi, do you run into problems with regulators or oversight committees?
Dingase Dula 26:01
There was no framework, right? We were the first group to introduce these trials to Malawi, there was no - I think - there was nothing to compare us against. And we sort of also built capacity in our local Research Ethics Committee. Because it's something that they didn't even, you know, consider they’d never reviewed or regulated these human infection trials. Even before we even started, we engaged - there were some of the first people that were engaged to say, look, we, in the next five years, we'll be doing these trials in Malawi, these trials are done elsewhere, but we want to start. If you were reviewing a human infection trial, what would you want to see? And actually, most of our procedures, like, for example, the quarantine, the tools that we use to ensure people are literate - you know, these were suggestions from the research ethics committee. So it's been a learning process for all of us, actually, we've moved together. Now they know about human infection trials. Now they actually, they know about all our trials. And you can see that for every trial we submit, some of the questions are kind of similar. They also grow, they're also learning, and you say, okay, they give us suggestions, and we’re like, ah, yeah, actually, yeah, we should, we should suggest that. You know, and so we're growing together with the research ethics committees.
Alisha Wainwright 27:18
So, as you grow and develop that capacity to do this research in Malawi, do you think you get the broader public to see vaccines as something that’s not just for kids, but for adults too?
Dingase Dula 27:31
Yeah, I mean, we, I think there's a lot of work that needs to be done. Yeah, there's a lot of public health messaging that needs to be done, because we - adults are not getting vaccines because we can't afford to give them the vaccines. Yeah. But we have adults that could benefit from these vaccines. So we need to really sit down and think of ways in which, when we find the interventions, how are we then going to make sure that people are accepting them? We don't want another Covid vaccine story, where we have lots of vaccine and nobody's getting, yeah? So I think it's an area that we really, really need to look at. And we need to transform people's way of thinking in the next couple of years.
Alisha Wainwright 28:20
So what's next for this pneumococcal vaccine? And what further study would you like to see?
Dingase Dula 28:26
We are actually now calling back the participants. For example, Becky and Stonard, they came the first time around, we give them bacteria. We're calling them back a year later, to re-challenge them with bacteria, again, to see - how is the protection one year later? Yeah. So that will inform even our vaccine strategy to say, okay, how are we supposed to give this vaccine? Is one dose enough? Should we be giving a booster? And at what point should we be giving a booster? So we, we're still, we're not done. We're not where, I don't think we're even halfway done with the work we're doing with this particular vaccine, even though it's already being given to children. So we hope that at the end of two to three years, we'll have, you know, very crystal clear answers to say, you know, maybe this is the dose of vaccine we need to be giving. Instead of one dose, let's give - every set of three doses, let's give maybe two doses at first, then another dose one year later, let's give it to this population. Or maybe let's give it again at this particular time point. So we want those crystal clear answers that we can give to policymakers so that they can, we can maximise the potential of this vaccine. Because it works, yes, but it could work better, we could get 80% efficacy, if we just study it closely in our population. So that's what we're doing with this vaccine. But what we're looking forward to next is TB, because TB is a very big problem here in Malawi.
Alisha Wainwright 29:48
Tuberculosis?
Dingase Dula 29:49
Yeah, tuberculosis, yeah. We only have one vaccine, which is given at birth, but the protection wanes very quickly, such that a lot of people get TB. So we are going back to the drawing board to say, how can we use these same concepts to design interventions for TB, or to understand TB better in Malawi? How can we eliminate TB? Because the WHO has set a target to say we would like to eliminate tuberculosis, you know, in endemic settings by 2035. Yeah. And there are so many public health strategies that are being put in place to eliminate - as well as clinical strategies. So we're now saying, how can we use our model human infection trials, to join this fight against tuberculosis in one way or another? So we're really forward looking to see, you know, just like the Liverpool group, are solving problems that are relevant to them. We are also looking forward to solving problems that are very relevant to us and TB is our next big challenge.
Alisha Wainwright 30:57
This conversation was so fascinating. I want to thank you so much for your time and your knowledge. I learned so much. And I'm sure everyone listening did as well. Thank you Doctor Dingase Dula, I really appreciate it.
Dingase Dula 31:12
You're welcome. You're welcome. Thank you for having me on the, on the podcast.
Alisha Wainwright 31:22
Thanks for listening to this episode of When Science Finds a Way. And thanks to Dr Dingase Dula, Becky Mkandawire and Stonard Mwale.
I learned a lot here about human infection studies from Dingase. Obviously it’s reassuring to hear how safe they are, but when we talked about the benefits of this locally-led research, with vaccines being tested and developed in the communities that need them most, I felt really hopeful for the future.
When Science Finds a Way is brought to you by Wellcome.
If you visit their website - wellcome.org, with two Ls – you’ll find a whole host of information about research into infectious disease, as well as full transcripts of all our episodes.
If you’ve been enjoying When Science Finds a Way, be sure to rate and review us in your favourite podcast app. And you can also tell us what you think on social media - just post on your socials and tag Wellcome Trust - that’s Wellcome with two Ls - to join the conversation.
Next time, we’ll be talking about research into ancient DNA – and the power of collaboration between scientists and indigenous communities.
When Science Finds a Way is a Chalk and Blade production for Wellcome - a global charitable foundation that supports science to solve the urgent health issues facing everyone.
Show notes
Vaccines are formidable tools against infectious disease. But the success of a vaccine in one part of the world doesn’t guarantee similar outcomes elsewhere. That’s where human infection studies come in – where volunteers, closely monitored by researchers, receive a vaccine and are subsequently given a small dose of an infectious disease. This might sound worrying, but it is a quick and effective way to get data about whether a vaccine is working.
Alisha speaks with Dr Dingase Dula, who researched a pneumococcal vaccine in Malawi, to learn more about the impact of infection studies. They also meet Becky Mkandawire and Stonard Mwale, who volunteered to take part in the study. They discuss the role of trust in human infection studies, what it’s like to be part of one, and the importance of African-led research in combating infectious disease.
Meet the guest
Next episode
Danish geneticist Eske Willerslev and Shane Doyle, a member of the Crow Tribe in Montana, USA join Alisha to discuss the possibilities and pitfalls of ancient DNA research, and how to build mutual trust and respect between indigenous communities and scientists.
Transcripts are available for all episodes.

More from When Science Finds a Way

When Science Finds a Way: Our podcast
Our podcast is back with a third season, uncovering more incredible stories of how scientists and communities are tackling the urgent health challenges of our time.