Episode 12: Will genomic sequencing prevent future pandemics?
Alisha speaks to Professor Christian Happi about his pioneering use of genomic sequencing during the 2014 Ebola outbreak in Nigeria, and how the technology could unlock the secrets of disease prevention.
Listen to this episode
Christian Happi 00:05
We are an endangered species, as humans, we’re in danger – especially because, if care is not taken, if you're not working together, we might end up getting extincted by these viruses or these pathogens.
Alisha Wainwright 00:20
This is When Science Finds a Way - a podcast from Wellcome about science that’s changing the world.
I’m Alisha Wainwright.
And this is where you’ll hear stories of hope - from people on the front line of our biggest health challenges.
And boy, am I bringing hope in spades today. In fact, it’s SUCH a fitting way to end the series, because we’re not only meeting someone whose work has changed the world - it may have just saved it.
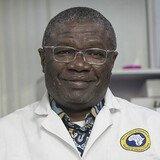
Christian Happi is Professor of Molecular biology and genomics at Redeemers University in Nigeria, and the founder and director of the African Centre of Excellence for Genomics of Infectious Diseases. Or, as he calls himself, a “pathogen hunter.”
Christian Happi 01:11
To contain an outbreak or an epidemic, you need two things: speed and accuracy.
Alisha Wainwright 01:17
Christian’s dedicated his life to understanding and hunting organisms that cause diseases, otherwise known as pathogens. As we heard earlier in the series, across the continent of Africa infectious diseases are responsible for around half of all deaths, and Christian sees these pathogens as a major threat to the human race. As he puts it, they want to get rid of us, so we need to get rid of them - or at least find solutions when they choose to attack us.
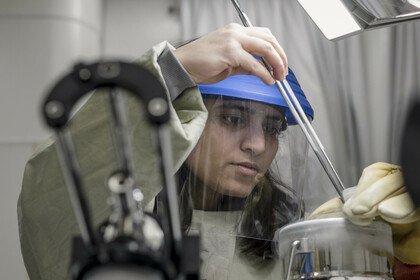
The secret weapon in his arsenal? Genomic sequencing. As Christian explains, it’s enabling us to UNRAVEL these pathogens. This means we can be on the offensive when they appear, but also - by investing in things like sequencing labs - we can better understand them, and shift the focus towards prevention. We’ll hear from a doctor in Guinea about how having in-country genomic sequencing was a game changer when ebola re-emerged there in 2021.
And what’s especially exciting, is that it’s scientists based in Africa - like Christian - who are pioneering the use of this technology. As you’ll hear, his team is changing the decades-long practice of western scientists parachuting in to “manage” disease outbreaks. Now scientists based in Africa are showing the world how to respond globally to pandemics and health crises.
Christian Happi 02:48
It makes no sense for, a disease to happen in Nigeria, and the diagnosis is done in London, or in Germany, or in the US. You’ve got to be on the ground to provide information, and that information has to be used on the ground to solve the problem.
Alisha Wainwright 03:00
I think this has to be one of the most positive and empowering episodes we’ve recorded so far - and frankly, I’m glad Christian is on our side in the war against infectious disease. Here he is to tell us why he’s dedicated his life to this cause.
Christian Happi 03:19
As a child, you know, I suffered from malaria. Growing up in Africa, I remember having one of the most difficult bouts of malaria in my life, when I was about maybe seven or eight years - I thought I was gonna die. And I remember my mum bringing me back from hospital, And at some point, she was tired under a tree, she stopped, and put me on the ground. And then I asked her the question - why am I this ill? And why is it that there is no cure for this disease? And her answer at the time was - I don't know. And I remember vividly telling her that look, when I grew up, if this disease is still around, I will find a cure for it. Yeah, I haven't found a cure for malaria, but I'm finding a cure for other things.
Alisha Wainwright 04:04
I'm sorry, I want to give the child in you just the biggest hug. That story is so moving, because it explains from even at a young age, your ambition to solve these intense, intense challenges. Let's start from a very basic ground level so that everyone can start to understand how you are combating pathogens. Can you describe genomic sequencing?
Christian Happi 04:34
Yeah, genomic sequencing is the ability to understand or elucidate, or to unravel or to break down the genetic material of an organism. And once you unravel that genetic makeup, then it provides you with endless possibilities. And these possibilities are your ability to use that genetic makeup to create drugs, even against that organism that you just saw unravelled its genetic material, to create vaccine against it, to create diagnostic, to actually to identify it. I think that's really the power behind genomics.
Alisha Wainwright 05:15
And when it comes to infectious diseases, what kind of information can genomic sequencing give us?
Christian Happi 05:24
When it comes to infectious diseases, genomic sequencing can not only help you to pull apart the engine of an organism, it can also tell you where the organism came from; it can tell you where it has been; it can tell you, what are the things that you need to suppress it?
Alisha Wainwright 05:43
That’s a lot of information.
Christian Happi 05:44
It's a lot of information. And actually, it gives you an opportunity to look deep inside an organism, and identify the weakest link, or the weakest point of the organisms, and now you're creating the tools that are needed in order to combat that organism.
Alisha Wainwright 06:06
Can you perhaps maybe give an example of where we've been able to sequence an infectious disease to maybe learn a little bit more about it?
Christian Happi 06:16
One example that I can use very clearly, and that is vivid in everybody's mind is the SARS-COV-2, which is the virus responsible for COVID-19, that the pandemic that we're all just, I mean, going out of. The reality is, you know, when it started, we didn't know which organism was responsible, but genomic sequencing enabled us to not only unravel, but actually to break down and then let us see all of the different parts of that particular virus. And because we knew what the virus was made of, we knew all of the different components of that virus, then we were able to, for the first time in the history of mankind, within months, to create a vaccine, that is quite a way of preventing the virus from spreading. So that's one example that can illustrate the power of genomic sequencing. But along the line, you know, we are able to use genomic sequence information to know the different type of viruses that were circulating at given times, in given places. So that also enables us to identify, that is to put like an identity on every circulating pathogens, know where they come from, where they were going, and then how they've been spreading around. So that does really give us also that opportunity to understand.
Alisha Wainwright 07:36
OK let’s hear now from someone on the ground. And I’m going to take you back to 2014. Ebola has hit West Africa - starting in Guinea at the very end of 2013 before quickly spreading to neighbouring Liberia and Sierra Leone. Doctor Sory Condé is an epidemiologist working in Guinea, who’s currently the head of the disease surveillance and response department, at the National Health Security Assembly. He told us what it was like back in 2014 at the beginning of the outbreak, when there was so little information known about the virus...
Dr Sory Conde 08:15
(French fading to translated voiceover)
We were always afraid, even colleagues going out in the field. We realised that the behaviour of some in our group sparked a kind of resistance in certain members of the community. There were false rumours going around, false information that we were the ones passing on some of these incurable diseases. That's what led some people to ask - if there's no treatment, then why should we go to a treatment centre? Isn't this just a way of getting rid of sick people? These rumours really worked against us. We came across an old health worker, an old nurse who had trained doctors in the past. He’d lost one of his wives, his mother in law and many of his children. But when my colleagues went there for contact tracing, he wouldn't come in, he wouldn't approach them. That's one of the things in a village like that. Families are ostracised, more or less, and therefore, they're not willing to work with us. We had to find smart ways to get them to work with us.
Alisha Wainwright 09:19
Wow. That must have been a really intense time, as we heard there was so much misinformation about how the virus was spreading, but sequencing can give us the facts, right?
Christian Happi 09:33
Absolutely. Because sequencing can tell you who has been in contact with who, who transmitted the infection to who, who contaminated who - lets me just put it in very clear term. And that's really what sequencing can do, you know, and give a clearer picture. And that really becomes important as a way to, you know, prevent, you know, further transmission.
Alisha Wainwright 09:56
Eventually, Ebola made its way to Nigeria, where you are based. And this is where your role as “pathogen hunter” really started to get going. You decided you wanted to pioneer something new - sequencing the virus in country, in real time. Which was something that was not typically done. Why did you want to do that?
Christian Happi 10:19
Why? Because we understood very, very early the power of genomics, because we understood that, if you had that ability, then you could easily - you could respond in real time, you could do what, you know, conventional epidemiology could not do in those days. And that's really what we shared with Nigerian government authorities at the time. They understood it, and that’s the reason why Nigeria was able to beat Ebola - I mean, within 93 days. A country of 230 million beating Ebola in 93 days with only 20 cases, and eight dead.
Alisha Wainwright 10:53
Wow. And I'm sorry, throughout this entire conversation, I will continually think back to the child in you, who had set out to embark on this journey. And here you are, that's so impressive. And this real-time sequencing, which again, was a world first, what did that tell you?
Christian Happi 11:13
It told us that, you know, you need a combination of technology innovation, to really beat a pandemic, it told us that, you know, to contain an outbreak or an epidemic, you need two things. One is speed, the speed of execution, two is accuracy, the accuracy of which you generate the information, and then you share the information, that is something that we took away from it, because you could - if you see the difference between Guinea and Nigeria during the pandemic, is the fact that in Guinea, it took time for them to confirm the presence of the virus. In Nigeria it took hours. So, within hours we knew - sharing information, also in real time became very crucial. And that's why we know and then we learnt from it that you need two things to beat an epidemic, you know, speed and accuracy
Alisha Wainwright 12:01
Speed and accuracy. And that played a major role in containing the outbreak. That makes a lot of sense. Also, after this outbreak, did neighbouring countries reach out to Nigeria to understand your response?
Christian Happi 12:17
It is very interesting to say that what we did in 2014 is what the world adopted in 2020, to respond to the COVID-19 pandemic. First, you know, using genome sequence data very quickly, reporting data in near real-time, right? And communicating information in real-time. Training public health workers on how to use these approaches to respond to epidemics. Identifying the viruses that transmit much more better from person to person. You know what, that's what we call “variant of concern”. We did that within the Ebola outbreak in 2014 in West Africa, so all of the things that we set up in 2014 is what the world used to respond to the COVID-19 pandemic.
Alisha Wainwright 12:59
Okay, so not only were lives saved from Ebola, but also this sort of downstream effect - snowball - if you will, of positive gains, because everyone is expanding on this level of knowledge. Okay, I'm going to try not to fangirl more, but I do want to ask, why was it important for this research to be done in country?
Christian Happi 13:22
It was important for the research to be done in country because it is the epicentre, that's where the disease happened. It makes no sense for a disease to happen in Nigeria, and the diagnosis is done in London, or in Germany, or in the US. You got to be on the ground to provide information, and that information has to be used on the ground to solve the problem. So in that doing, you are not only helping the immediate community or the country, they're also helping the globe.
Alisha Wainwright 13:48
Do you know why this had been the case? Why was it that outside forces would touch down, usually from Europe or North America, and come and take samples out of the country? Why would they do that? And furthermore, why was that problematic?
Christian Happi 14:05
First of all, they were doing it because they had this ill-conceived idea that Africans could not do things, or that people could not do things. They have this ill-conceived idea that nothing good can be done on the ground. And then this whole idea of controlling, you know, data, controlling samples. I didn't have a, what I call a high containment laboratory to do it, I did it in a place where you can work [on] malaria. And then I was able to share the information in real time to demonstrate that what could be done in Oxford, in London, or in New York, or, or in Sydney, or in Tokyo could be done on the ground in Africa. And that demonstration became very important in the sense that, you know, working with the locals, who, most of the time, understand the local situation better than those that are parachuting themselves, you know, is actually much more better for the rest of the world.
Alisha Wainwright 14:54
I will say, you know, I've been doing this podcast for a little while now. And I am continually impressed by this central idea of the people who have boots on the ground, know far more than anyone who is parachuting in from somewhere else, trying to learn information in real time. It's such a waste of time, rather, not just rely on the people who are there who are experiencing it, who know what is best, because they're there right now. And another thing you pointed out that I just want to ask for a little bit more clarity, you said outside countries would come in and control samples. What do you mean by that?
Christian Happi 15:30
What used to happen is that the “expert”, in quotes, used to come and then they will take all the samples to the laboratory in the US, or in the laboratory in the UK. In the name of biosecurity, in the name of biosafety, I'm not saying that it's not important. But at the end of the day, the countries, or the real owners of the sample lose absolute control of the sample, they lose everything about the sample, they don't know what comes out of it. They don't know exactly what is the outcome of those diagnoses, maybe they have been told. But then at the end of the day, they lose everything in terms of understanding the biology, understanding exactly what is the root cause, and they see the relationship, you know, between the sample and then the people. So I think by doing it on the ground, we just do two things, not only we were able to understand exactly what those samples are made of, but it's also empowering the local people so that tomorrow they can actually do things by themselves. You could see exactly how Africa handled the COVID-19 pandemic, it was true a sense of empowerment, because people could do things on their own, people can handle things on their own, and then they could respond much more better.
Alisha Wainwright 16:34
Guinea is also working to build its own in-country capacity to carry out sequencing. And while it wasn’t in place for the 2014 ebola epidemic, when there was a re-emergence of the virus in 2021, most of the sequencing was done locally. Here’s Dr Sory Conde again, to tell us more….
Dr Sory Conde 16:57
(French fading to translated voiceover)
For the second epidemic we carried out the sequencing, we realised that the virus didn't come from wild animals. It was the same strain as that of the previous epidemic. Given that we had Ebola survivors in the community, that implied that if it didn't come from wild animals then the virus was born from human to human transmission. And studies showed that the case of a woman who had triggered the process of notification came from a village in the Nzérékoré Region region, a village which had been particularly impacted by the epidemic. That gave us an inkling that the people who’d recovered from Ebola, even though it had been in 2014, and now 2021, so at least seven years, the virus could be reawakened at any moment. So because of that, we vaccinated people in the Nzérékoré prefecture, to improve the immunity of the population, especially people who had been in contact with the disease, people who tested positive, people on the frontline, health workers, port workers who had been exposed, people from the Red Cross. We did that in the Nzérékoré prefecture to bring the epidemic under control quickly. After that, we rolled out the preventative vaccination programme to the five other prefectures in the Nzérékoré region. At the beginning of the first outbreak, we said that the virus could be stored for three months in the bodily fluids of the person who had recovered from Ebola. When they left the treatment centre, we were educating them to say - you're well again, but you could transmit the disease to anyone you have sex with. Because of that, we recommend that you don't have sex for three months. But there were studies that had been done, which showed that the three month period was incorrect, the virus could last longer than that. The 2021 epidemic showed that it could hang around for more than seven years.
Alisha Wainwright 18:57
Wow. So in this instance, the sequencing led to a vaccination campaign to contain the outbreak. And the discovery that the virus could lie dormant in someone for that long, is also changing the public health messaging, you know, being given to Ebola survivors. So everything's happening - basically, as soon as the information is being understood, it's being translated to the community.
Christian Happi 19:23
Oh yes, you can see here, Guinea didn't have to send a specimen to France, for this analysis. So there is a gain here in time. And then you can see here, speed of our understanding the process, and also speed of response. And then also accuracy in the sense that they could see exactly where it came from. And also compare that with the 2014, and say, it is the same, which means it is from people, and the virus has been dormant in those people. So I think, though, I mean, it gets down to what I said before; speed and accuracy.
Alisha Wainwright 19:52
Can you give us any other examples of where your on the ground sequencing has helped contain an outbreak?
Christian Happi 19:59
Yes, I have several examples, but I can just take one, just to list. I mean, I have several. In 2018 - in November to be precise - within a week 176 children died in a rural community in Nigeria by, you know, a “mysterious”, in quotes, disease. The National Centre for Disease Control in Nigeria, they did an investigation, they tried to confirm whether it is Lassa fever, whether it is Ebola Virus Disease, whether it is malaria, or they’re common diseases that we know. They all turned out to be negative. They sent 22 samples to my lab, and within 72 hours we unravelled the fact that that outbreak that killed 176 children is due to a yellow fever strain that is very different from the one that has been circulating in Nigeria for the past 96 years to be precise. We make that information immediately available to the National Centre for Disease Control in Nigeria, and then they declare an outbreak in the region. And then they go into that region with the National Primary Health Care Development Authority. They go in and do a mass vaccination campaign for yellow fever. And then within two weeks the outbreak is contained and thousands of lives are saved.
Alisha Wainwright 21:20
Wow. That’s another great example of where both speed and accuracy have been essential in helping you contain an outbreak. And I know you’ve gone on to set up a global project called Sentinel, based on these principles. Can you tell me a little bit more about Sentinel and the role it plays in responding to outbreaks?
Christian Happi 21:42
Sentinel is an early warning, you know, system for pandemic preemption and response. Sentinel is actually based on my life experience working in the field, taking you know, lessons from what happens in the field. It is built on three major pillars. One is early diagnostics - that is, you know, detect pathogens using technology, early enough before they come to us as a people. That is putting the diagnostics in the hands of the rural people in the most remote places in the world, where they can detect a virus or a pathogen within an hour. So that gives you the ability to detect early. And if it is negative and [? 19:10], we take it to a sequencing hub where we can now detect if it's a new virus, or a new, like, SARS cov-2. And we can also use that genetic makeup of the virus to create a new diagnostic within two weeks. What is unique about Sentinel, is that as we are testing, we're also reporting the results of the testing real-time to national public health institutions.
Alisha Wainwright 22:53
So everyone's on the same page?
Christian Happi 22:56
Everyone is on the same page at the same time. And that is the second pillar, which is connecting, you know, National Public Health in real-time. That is the second pillar: connect. The third pillar is - empower, that is empowering our healthcare workers, those who are already in the trenches, in the field, on how to use these technologies. So it is built on those three pillars: detect, connect and empower.
Alisha 23:18
It’s almost like a circle
Christian Happi 23:20
It is a circle. But what is critical about Sentinel, is the fact that it's actually the background and what holds it is actually speed and accuracy.
Alisha Wainwright 23:30
Hmm. That's a very, very well thought out plan. And how long has this programme been live?
Christian Happi 23:36
We launched the programme in January 2020.
Alisha Wainwright 23:40
[laughs] couldn’t have picked a better time.
Christian Happi 23:43
Exactly, we didn't know that the world was going to be facing a COVID-19 pandemic. But what is interesting about Sentinel is that it demonstrated its ability and the capacity immediately, because by the time the US was struggling with obtaining diagnostics for COVID-19, countries like Nigeria, in Africa, Senegal, Sierra Leone, Liberia, where we're operating Sentinel, had diagnostics at hand. Nigeria is the first country in Africa to unravel the genetic makeup of the virus, because of the presence of Sentinel in the country. The good thing about Sentinel is also the fact that we shared our protocol to the rest of African countries. And you could see South Africa going on later on to discover their Beta variant. You know, you could see South Africa and Botswana going on later on to discover the omicron, you can see, you know, Africa also ramping up its testing capacity and its sequencing capacity. Sentinel, within the past two years, for instance, we were able to train people from 42 different African countries - Africa is made of 54 countries - that is more than two thirds. We're also able to support sequencing in 38 different African countries. And all of these data were used to help Africa respond in the most effective and efficient way to the pandemic within the continent. From the end of 2020, Africa had only about 5000 sequences, but because of the very strong training programme, by July 2021 Africa had more than 100,000 sequences. It shows the power of Sentinel, and that really helped Africa to ramp up in response to COVID-19.
Alisha Wainwright 25:22
Wow, OK, as someone who lives in the US, I was aware of South Africa sequencing the Beta COVID variant. But it’s wild to have the context of Sentinel and how it played a part in enabling this to happen. Especially given that you had only launched it a few months before.
You talked about how empowering healthcare workers is one of your pillars at Sentinel. They obviously play a critical role on the front line in any outbreak. Can you just explain what role they can play in sequencing?
Christian Happi 25:59
Right, let me put it in context, a healthcare worker in a rural community sees a patient or a child that is having a bout of fever, that is not resolved by any antibiotics or any antimicrobial, or any anti-malaria drugs. That healthcare worker suspects that it is something that is a bit strange. And then the healthcare worker will send a sample to a sequencing centre. That information is very critical, because you could see the healthcare worker providing the information, and then having a feedback immediately, that healthcare worker used that information to actually act on the ground, because you will know what to do. The next step is - I need to isolate this patient, I need to make sure that, you know, not many people come into contact with this patient because I'm dealing with a disease that is very transmissible and very dangerous. That is exactly the power of bringing genomic very close to the healthcare worker, and having the healthcare worker understand exactly what genomic can help him do in his practice.
Alisha Wainwright 27:07
So, before Sentinel, and before this sort of circle, when a healthcare worker came across a patient that was presenting in a way they didn't understand, what would they have done?
Christian Happi 27:21
They just go by guessing, and usually by guessing they may not get it right. And when you don't get it right, unfortunately, if it is a transmissible disease, then transmission is ongoing, and is occurring in a community.
Alisha Wainwright 27:33
So how does this idea of empowerment and connection and participation, how does that extend to the wider local community?
Christian Happi 27:44
It’s extending to a wider local community because within Sentinel we have an education programme, where you empower people. And then, guess what? The reason why we call it Sentinel is because we believe that if everybody is educated, if everybody understands the value of reporting whatever you see that is suspected in real-time to the community healthcare worker, then you are what you call a sentinel. The whole idea of Sentinel is actually to make every citizen a sentinel for the world, whereby whatever you see it, you report it, whatever you suspect, you report it, and then together we can act to prevent it from arising or spreading.
Alisha Wainwright 28:21
It takes a village.
Christian Happi 28:22
Yes.
Alisha Wainwright 28:24
In Guinea, this idea of community collaboration is also important. Here's Dr. Sory Conde, again.
Dr Sory Conde 28:33
(French fading to translated voiceover)
In the 2021 episode, it was a member of the Ebola Survivors Association who raised the alarm. And that was confirmed by members of the family. It's so important, therefore, that the community can work with everyone who's been through the experience. Ebola survivors, their parents, their contacts, their associates, and the whole community can help us detect it more easily. The faster we can detect it, the less the damage. And the quicker we can come out of the epidemic. Look what happened in 2014, how much time did it take us? More than two years. But in 2021, it took us four months and a few days. So even in terms of the numbers of death, that wasn't the same. In the first outbreak, we had to send the samples to France, to Lyon, to find out what it was. The disease was spreading, and we didn't even know what it was. And if you don't know your enemy, you don't know how to fight it. That took up a lot of time. Whereas in 2021, the lab workers had been trained, the labs were equipped so that we could identify the virus that was triggering Ebola. And in no time at all, confirmation had come back from the laboratories and the sequencing had been done. We knew what we were dealing with. We knew what the enemy looked like, how it was transmitted, and so on, and even what type it was. So today, we continue to improve so that we can sequence Ebola, we can sequence COVID-19, to know which variant it is. We're working to acquire the technical know-how and strengthening the skills of the workers so that we're in a better position to do it for the whole range of pathogens that we see here, in order to minimise the effects of any outbreak.
Alisha Wainwright 30:23
What's your takeaway from hearing Sory?
Christian Happi 30:26
I think the takeaway is clear. They learned from the 2014 outbreak, the world learned from what we did to save Nigeria, and then that's what they apply. And then you can see here, it comes back to two things: speed and accuracy. As I mentioned before, I mean, they did it in a very short time, they had a sequence, and then we were able to address it. It is the same thing, bring it in the context of the COVID-19 outbreak, and that gave the impetus and the confidence to everybody in Africa that we could do it, and that you could see Africans responding to it because they saw it done somewhere within the continent to the Sentinel programme. And then they could replicate that. Sentinel really had this huge impact on the continent, to the capacity building programme. And that's why, you know, without discrimination, we've been able to achieve and impact 42 out of the 54 countries in Africa.
Alisha Wainwright 31:19
Without discrimination, yes.
Christian Happi 31:21
Yes, and we're hoping to actually close on a map of Africa, you know, by the end of this year.
Alisha Wainwright 31:27
And, you know, which countries have been leading sequencing? And what can the rest of the world learn from them?
Christian Happi 31:37
South Africa has been a great example, Nigeria has been a great example to the to the Sentinel programme, you know, discovering the beta variant, discovering the omicron variant and discovering the eta variant that we discovered in Nigeria, showing that you know, those variants emerge from here and then spread. But then what is great about Africa is the fact that, as we discover these variants, we share with the rest of the world. We created and we pioneered open data sharing, open data access, you know, and make information available to the, to the global health community. So that this information can be used to address issues like diagnostics, vaccine, or therapies. But unfortunately for us, by making, by sharing this information, many countries in the Global North use that as a way to stigmatise us, to say - oh, wow, this variant is coming from South Africa, this variant is coming from Africa. Remember, when South Africa reported the beta variant, what happened? They ban Africans from travelling, because they thought that they were bringing this variant. And yet it was just for global public good that we were sharing this information.
Alisha Wainwright 32:40
Right, I see. What are the risks of the global community responding in this way?
Christian Happi 32:47
By stigmatising Africans the way they did during the COVID-19, then they create a situation whereby in order to avoid stigmatisation in the future, people may not be willing to share information every time. That is a very big public danger. So there is definitely, you know, a loss of trust from the, I mean from Africans, because if you are sharing information, and then you know that that information will be used to stigmatise you, why do you go ahead and share it? So I think there was a big disservice by the Global North, in stigmatising African countries for sharing information, or for doing what is right. So I think there is a need to, to change the narrative and to do things right, you know, going forward, and give confidence in people by letting them know that - you know what, going forward, if we share information, you're not going to be stigmatised or you're not going to be sanctioned for doing the right thing.
Alisha Wainwright 33:40
What's your vision for the future of global disease outbreaks and how they can be managed?
Christian Happi 33:46
Well, I do think that, you know, the future should be about creating a community of good practice, getting people to work together. And then you know, I mean, refrain from stigmatising people for sharing information, and also investing, let's invest in the places where the risks are high in periods of peace. Let's get prepared. So that when there is a potential outbreak, then we’re all prepared and all equipped and ready to fight the outbreak. I always refer to Nigeria - how a country of 230 million people beat a disease that is as deadly as Ebola, in 93 days, with only 20 cases, is simply because they were prepared. We had a diagnostic in place, we had ways of sequencing in place, we had a health sector that was prepared, there was a cooperation between the private sector, the government and then all of the actors in the country were involved. So as a global community, as a people, we need to cooperate, we need to work together as one people in order to address this whole challenge of infectious pathogens. Because I always say, you know, we are an endangered species, as humans we’re an endangered species, because if care is not taken, if you're not working together, we might end up getting extincted by these viruses on these pathogens.
Alisha Wainwright 34:59
Are we our own enemy in this, in terms of getting everyone on the same page about being informed and having the right diagnostics in place?
Christian Happi 35:07
I do think so, and then we should stop politicising these things. Let science do its own thing, let public health function globally as a way it is.
Alisha Wainwright 35:15
Less politicising of science - I 1,000% stand behind that. I think we would accomplish a lot more if there was less of a feeling associated with these facts.
Thank you so much for your time, and your hard work. And I really enjoyed this conversation. Thank you.
Christian Happi 35:35
Well, thank you very much. And then thank you for the opportunity given.
Alisha Wainwright 35:40
Thanks for listening to this episode of When Science Finds a Way. And thanks to Christian Happi, and Dr Sory Conde.
I’ve left this conversation feeling so positive and empowered - so Christian’s pillars are clearly working on me! He’s got such a clear plan which makes total sense for expanding on a global level, and we all need to take a minute to recognise the influence that his work in Africa has had across the world. There were many amazing genomic initiatives utilised during the COVID pandemic and Sentinel was certainly one of them.
When Science Finds a Way is brought to you by Wellcome.
If you visit their website – wellcome.org – that’s Wellcome with two L’s – you’ll find a whole host of information about infectious disease, as well as full transcripts of our episodes.
If you’ve been enjoying When Science Finds a Way, be sure to rate and review us in your podcast app. And you can also tell us what you think on social media - just tag Wellcome Trust - with two Ls - to join the conversation.
This is the last episode in series one! Thank you so much for listening, and stay subscribed because there is a bonus on the way… so it’s not quite over yet.
When Science Finds a Way is a Chalk and Blade production for Wellcome – a global charitable foundation that supports science to solve the urgent health issues facing everyone.
For Chalk and Blade, the producers are Katie Bilboa, Matt Nielson and Rosie Stopher, the showrunner is Sarah Stolarz and the executive producers are Laura Sheeter and Ruth Barnes, with mixing and sound design by Matt Nielson. Original music is by MARO and Nico.
Thanks also to everyone at Wellcome who has contributed to the making of this podcast - there’s a huge team behind the series and we couldn't have done it without you.
Show notes
During the Covid-19 pandemic, the benefits of sequencing infectious disease pathogens became more visible than ever before. The possibilities are huge: genomic sequencing is allowing scientists to unlock the secrets of disease prevention, helping dispel myths and stigma around disease outbreaks as well as allowing governments to act in real-time with targeted and often low-cost interventions.
In this episode Alisha speaks to Professor Christian Happi, Director of the African Centre of Excellence for Genomics of Infectious Diseases, about his pioneering use of the technology during the 2014 Ebola outbreak in Nigeria which identified the origin of the virus. They hear from the lead researcher who used sequencing to map a subsequent outbreak in Guinea, changing how healthcare workers understand the disease.
Meet the guest
Next episode
Join Julia Gillard, Chair of Wellcome, as she brings together three experts from the series to reflect on the main themes that have emerged and ask what challenges still lie ahead in the field of global health.
Transcripts are available for all episodes.

More from When Science Finds a Way

When Science Finds a Way: Our podcast
Our podcast is back with a third season, uncovering more incredible stories of how scientists and communities are tackling the urgent health challenges of our time.