Research is saving lives in the Ebola outbreaks in DRC
Protecting the people of the Democratic Republic of the Congo from Ebola takes a chain of responders from all over the world. With one outbreak earlier this year over, and a second ongoing, research has been at the heart of the response.
On 8 May 2018, the government of the Democratic Republic of the Congo (DRC) confirmed an outbreak of Ebola virus in the country, in the Équateur Province. DRC had already contained several outbreaks of Ebola since the virus was first identified there in 1976. But following the 2014-16 outbreak in West Africa, in which more than 11,000 people died, it became clear that Ebola had the potential to cause a deadly epidemic.
On the day Ebola was confirmed, Wellcome released £2 million to fund research in DRC that would support the emergency response. The UK Department for International Development gave a further £1m via a partnership with Wellcome, the Joint Initiative on Epidemic Preparedness.
The rapid response from a range of organisations across the world was vital to containing the outbreak. Out of 54 cases, 33 people died, which was on a similar scale to the three previous outbreaks in DRC between 2008 and 2014.
On 1 August 2018, a week after the Ebola outbreak that had begun in May was declared over, another began. This time it was in DRC’s North Kivu province. Containing this ongoing outbreak is proving much more challenging and complex.
It’s in a densely populated urban area, making transmission more likely. And some of the cases reported are in areas where there are armed conflicts, making it difficult for researchers and healthcare workers to provide care, gather data and trace the virus effectively.
With over 450 confirmed and probable cases, this is now the second biggest Ebola outbreak in history.
Wellcome has released more funding to support the response on the ground.
So what research has been supported in DRC, and how will it help halt the ongoing outbreak and prepare us for future epidemics?
Vaccination
For the first time, an Ebola vaccine was available at the start of an outbreak. The vaccine, rVSV-EBOV, is manufactured by MSD (Merck). Many people have been involved in its development, from researchers at the Public Health Agency of Canada to pharma companies, governments and NGOs, as well as the scientists and medical teams who ran clinical trials and the volunteers who took part in them.
Wellcome played a role, too, funding research and pushing for clinical trials to be done during the 2014-16 epidemic. These trials, coordinated by the World Health Organization (WHO), showed that the vaccine was safe and effective.
rVSV-EBOV has not yet been licensed, meaning that it can only be used in research studies when consent is obtained from the people taking part and they are followed up to monitor safety.
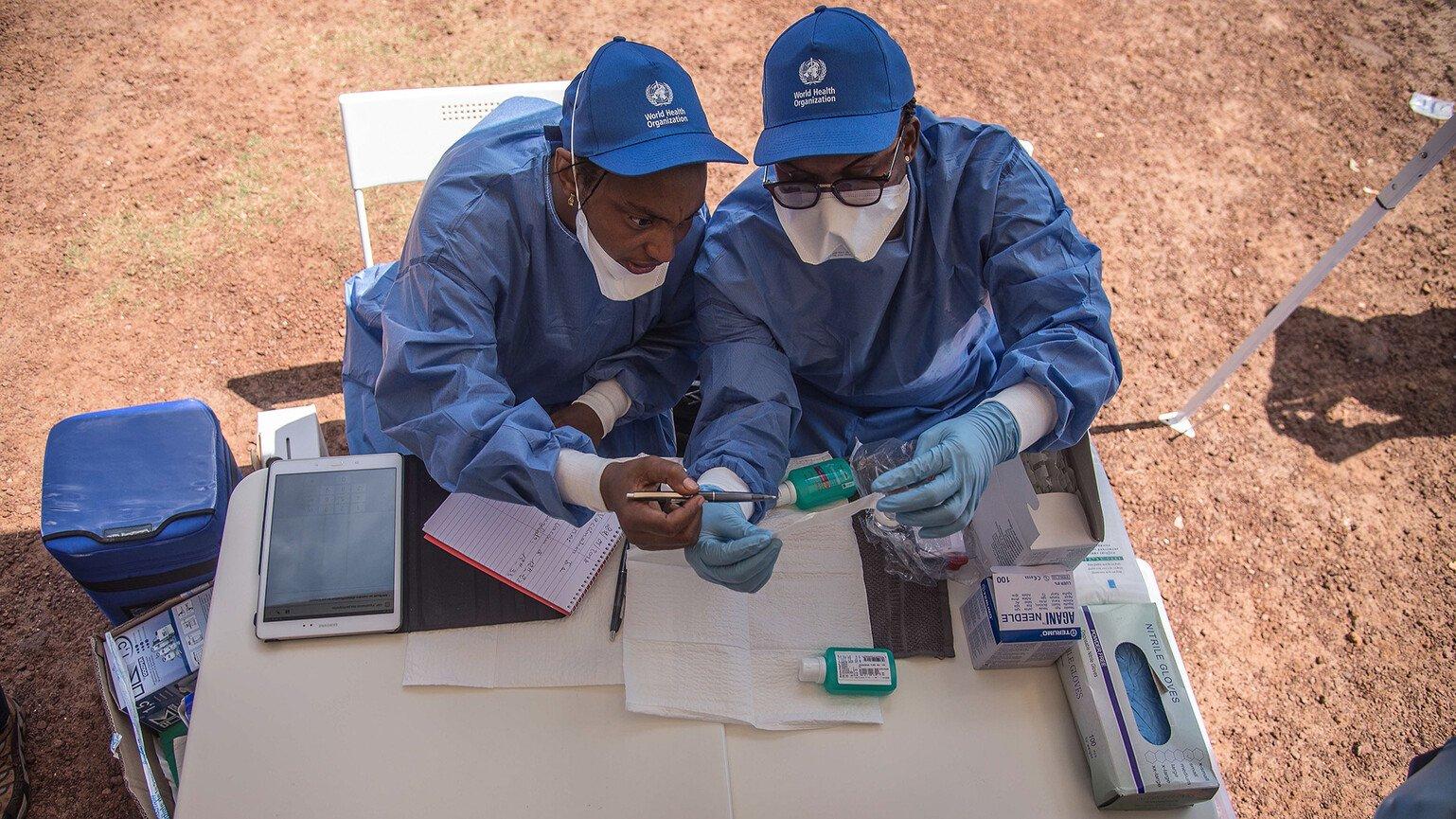
But with our research funding in place, the DRC government, WHO and Médecins Sans Frontières quickly began setting up a vaccination programme in the Équateur Province. This involved bringing in freezers to store the vaccine at -70°C, hiring the people who would do the fieldwork, and working with other partners such as UNICEF to engage the communities who were at risk.
Experts from Guinea shared their first-hand experience of the ‘ring vaccination’ approach and good clinical practice when caring for people with Ebola. Ring vaccination means identifying everyone who has been in contact with an Ebola patient, and then in turn tracing everyone the people in that first ‘ring’ have been in contact with. Everyone in these rings is offered the vaccine, as well as first responders such as health workers and taxi drivers.
During a crisis, this is a more practical approach than trying to vaccinate an entire population. But it still relies on epidemiologists, lab workers testing samples, and thousands of personal visits by trained contact tracers.
Between May and July 2018, more than 3,300 people were vaccinated in the Équateur Province.
The vaccination programme may have helped to slow and even stop the spread of the virus. But it is hard to draw any firm conclusions because the outbreak was relatively – and thankfully – short.
It’s been much tougher to deliver vaccination in DRC’s North Kivu province because of the ever-present threat of violence, and the distrust some of the local communities have of health officials.
Despite these obstacles, so far 40,000 people have been vaccinated using the ‘ring vaccination’ model. As a result, we will learn more about the vaccine’s safety.
Clinical care
People with Ebola need to be able to trust that they will get the best possible care, and the best care starts with the right diagnosis. In its early stages, Ebola tends to involve a fever, aches and pains – similar to infections like malaria or flu.
During an epidemic, it’s vital to know who actually has Ebola before they develop life-threatening symptoms, including vomiting, diarrhoea, organ failure, and internal and external bleeding.
Some of Wellcome’s funding went towards building up DRC's capacity to use and assess new and developing diagnostic tools in outbreaks.
A handful of drug treatments for Ebola are in development – again, none of them has yet been licensed, so WHO and DRC authorities agreed protocols for using them on a compassionate, case-by-case basis.
The first outbreak was over before any of them were prescribed. With the current outbreak, it quickly became important to move from compassionate use to a randomised controlled trial of the existing drugs. The trial will help researchers collect data to find out if any of these treatments save the lives of patients with Ebola. Collecting this data wasn’t possible when using the treatments compassionately.
Designing a trial for the North Kivu outbreak has been particularly challenging because of the local conditions. Wellcome’s Director, Jeremy Farrar, has co-chaired the WHO Ebola Therapeutics Group responsible for overseeing this work.
The multi-year trial, sponsored by Congo’s National Institute of Biomedical Research, started in November, and will span several outbreaks and countries. This is a key moment in developing a treatment for Ebola which could turn this deadly disease into a treatable one.
Communication, coordination and capacity
Epidemics are alarming and frightening wherever they happen. It's vital that communication between officials and the public is constructive, that research is supported, coordinated and shared, and that people feel engaged with decisions that get made.
Wellcome funded a team to produce operational briefs setting out local social and cultural contexts for both outbreaks. These helped shape communication with affected communities about Ebola, the vaccine and other public health measures.
Some of Wellcome’s funding has been used to strengthen research capacity in DRC so that the country is better prepared to respond to outbreaks, facilitating research on Ebola now and in the future.
This includes support for the National Regulatory Authority and the Ethics Research Committee, and establishing a national research coordinator at the National Biomedical Research Institute (INRB) in Kinshasa.
Preparation
Ultimately, the effect of quickly committing funding has been to ensure that research is integrated in the emergency response to the Ebola outbreak, led by the DRC government with support from WHO and other partners.
Epidemics are not single events. Every nation around the world needs to know their risks – some have to deal with seasonal epidemics, others with sporadic outbreaks, but all have to be ready with robust plans in place.
And, crucially, research needs to be an integral part of these plans so that we learn more from every outbreak and become better prepared for the next one.
Related links
- Find out more about our work to equip the world for fighting infectious diseases through our Vaccines priority area
- Why do we need vaccines?