Eight cutting-edge immunology projects we fund
29 April is World Immunology Day 2018. Divya Shah and Pete Gardner, from our Science team, highlight some of the researchers we fund who are exploring different aspects of immunology and the immune system.
The immune system underpins our body’s ability to fight infections and heal itself. Understanding how it works could lead to new treatments for a wide range of health conditions, from autoimmune diseases like diabetes and multiple sclerosis, to life-threatening or debilitating allergies.
The following eight projects highlight the diverse range of research that Wellcome funds in this area.
The 3i project: immunophenotyping
The 3i project is all about scale. Its ambition is to build a free encyclopaedia of immunological gene function that will allow new questions to be asked in both basic and applied research for years to come.
The project is a collaboration, led by Professor Adrian Hayday, that involves research centres across the UK and USA. It uses mouse knockout lines generated by the Wellcome Sanger Institute as part of the International Mouse Phenotyping Consortium to look for genes that regulate the immune system during both health and illness.
Over 20% of the genes identified so far have an impact on the immune system, many of which were previously not known to play any immunological role.
The team has also created a website that makes their data freely available for other researchers to use.
Calliope Dendrou: the genomics of autoimmune disease
Autoimmune diseases affect hundreds of millions of people worldwide. They are on the increase, particularly in developed countries, and there are currently no cures. And although there are many possible factors that can initiate disease, such as genetics, the environment, and infections, it’s not yet clear exactly how this is happening.
Seeing what happens when the immune system goes wrong is also a great way to start figuring out how something so complex and multi-layered works.
Calliope Dendrou is a Sir Henry Dale Fellow based at the Wellcome Trust Centre for Human Genetics in Oxford. She is looking at the shared genetics of autoimmune diseases such as multiple sclerosis, Type 1 diabetes and rheumatoid arthritis.
Calliope has shown that data from genome-wide association studies (GWAS), which links particular genes with particular traits, can be used to find drug targets and potentially lead to new therapies that could be used to treat more than one autoimmune disease.
Sophie Hambleton: cohorts to study autoimmune disease
Patient cohorts are a valuable tool for immunologists.
Sophie Hambleton is Professor in Paediatrics and Immunology at Newcastle University. As a clinican, she has access to a large paediatric cohort to help her explore what is happening when the immune system malfunctions.
With next-generation sequencing technology, she's able to look at mutations in the genomes of children with autoimmune diseases, and in some cases their families’ genomes to help understand inheritance of disease.
By identifying new genes involved in the early stages of disease, she can study the molecular pathways that may lead to new and improved therapies and diagnostic tools for patient benefit.
Becca Asquith: maths to overcome the limitations of animal models
Wellcome is always interested in interdisciplinary approaches that use physical sciences, including maths, to explore biological questions.
Becca Asquith has an Investigator Award and is a Reader in Mathematical Immunology in the Department of Medicine at Imperial College London.
Her award focuses on the role of receptors on natural killer cells, a class of white blood cell, and their role in how the immune system responds to viral infections. Becca looks particularly at a receptor called a killer-cell immunoglobulin-like receptor (KIR).
KIRs are significantly different in humans as opposed to mice, and so there’s a limit to what can be learned using mouse models. Becca uses a mixture of mathematical modelling and experimental approaches to overcome these limitations.
Eric Schockmel and Megan MacLeod: Immunecraft, a multiplayer video game
Eric Schockmel and Megan MacLeod formed an artist/scientist collaboration for Silent Signal, an experimental animation project.
Eric is a moving image artist and director based in London. Megan is a Lecturer in Immunology at University of Glasgow, researching the immune system's 'memory', which allows some white blood cells produced in an immune response to protect against future infections.
They created Immunecraft, a trailer for a fictional multiplayer online video game that explores cellular immunity by giving players control of white blood cells in a battle against infection controlled by opponent players. The game looks at themes such as how cellular soldiers coordinate defence, and track down and engulf invading pathogens.
Marta Polak: environmental causes of allergic reactions
Allergies are common worldwide and an increasing problem. We’re now starting to understand more about how allergies develop and the importance of the environment's impact on our immune system. This knowledge may lead to us understanding more about how we can better treat allergies.
Marta Polak is a Sir Henry Dale Fellow, working at Southampton University. Her focus is on the critical role played by Langerhans cells, a particular type of immune cell found only in the skin, and their involvement in triggering allergic reactions. This may lead to new drug targets that help patients tolerate allergens.
Dan Davis: immune synapses revealed by new imaging techniques
New imaging technologies are opening up areas of science for researchers to explore.
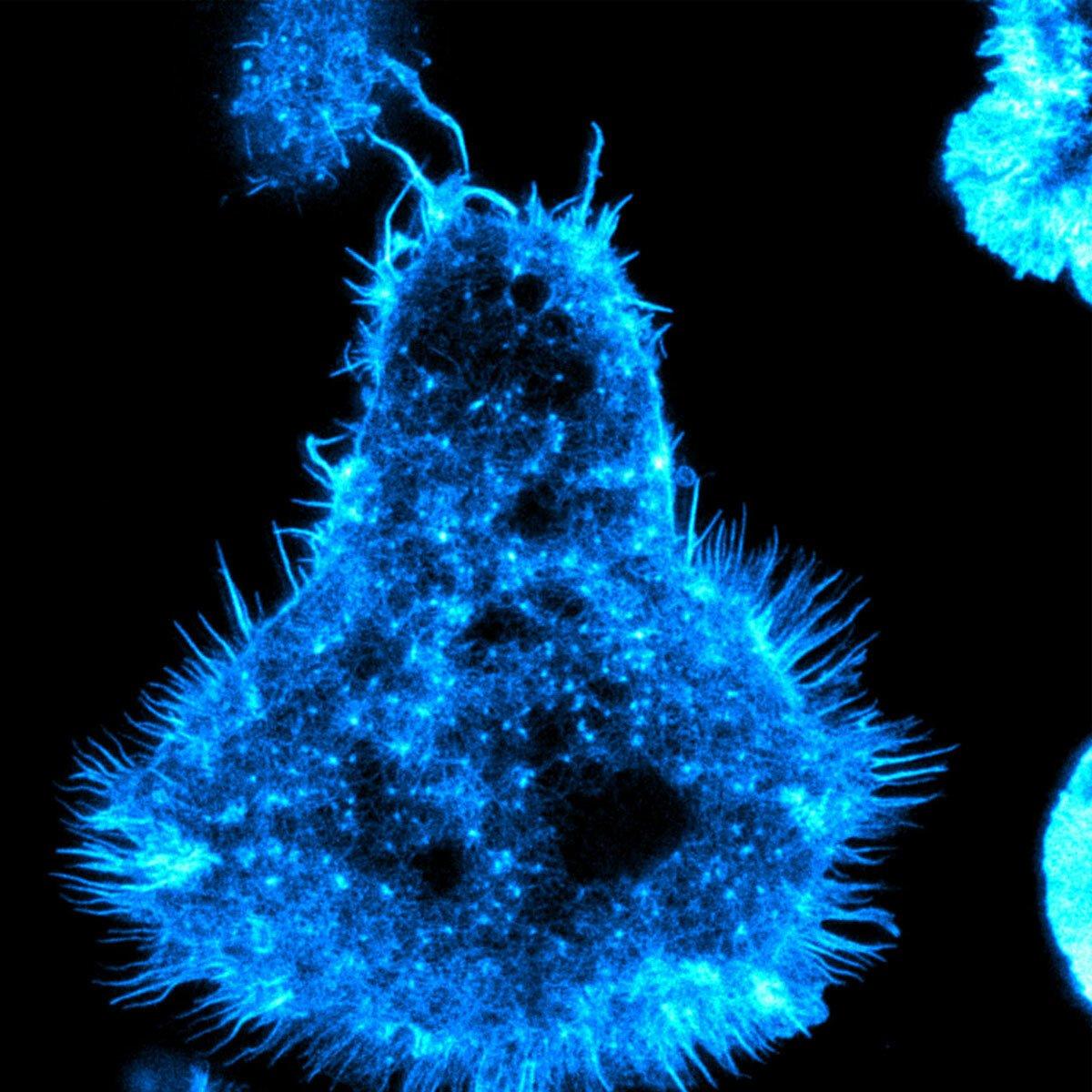
Dan Davis is Professor of Immunology at Manchester University, and has a Wellcome Investigator Award. He’s taking advantage of recent improvements in high-resolution imaging to look at how the cell membranes of immune cells physically contact one another – what’s known as the immune synapse.
This is revealing the intricate way that cell membrane proteins organise into micro clusters within these synapses and facilitate transmission of signals between two cells. This type of cellular communication is vital in determining if and when white blood cells are activated as part of the immune system.
Graeme Meintjes: patients in low- and middle-income countries
We fund an increasing number of researchers in low- and middle-income countries. Supporting world-class research in regions that face some of the greatest health challenges will have a major impact on health outcomes.
Graeme Meintjes is Professor of Medicine at the University of Cape Town and a Wellcome Public Health and Tropical Medicine Intermediate Fellow. He focuses on groups of patients with multiple infections who are very difficult to treat.
Graeme is currently leading a study of patients infected with HIV who are also hospitalised with tuberculosis. His team is investigating what might lead these patients to die, such as the reactivation of latent viruses, or the damage caused by their own immune responses.