
Drug-resistant infections: the science is on track, but the economics need fixing
Thousands of lives around the world could be saved every year if we can develop new antibiotics to treat drug-resistant infections. The problem we need to fix is how to make antibiotic research and development sustainable.

Luuk Rombouts / Ideo. All rights reserved
"There were antibiotics that I was using when I first came into practice, and we were confident they would treat most infections. The resistance to those antibiotics is now very significant, about 30% in some regions in the UK."

Berit Muller-Pebody, Antimicrobial Resistance Section Head at Public Health England, adds: "It is a pressing and very worrying trend. We already treat many with our last resort antibiotics, and now we see resistance emerging to these."
The obvious solution is to come up with new drugs, but antibiotics are so unprofitable that big pharma has all but pulled out of the market. Some small companies have made exciting breakthroughs on developing new classes of drugs but face massive financial barriers in getting these new antibiotics to doctors and the patients that need them. The science is starting to work, but the economics need fixing.
Santanu Datta, Chief Scientific Officer of Bugworks, states: "There is a financial problem, but the unmet need is so huge. People are dying. You cannot put a price on people’s lives."

Discovery – the basic science
The World Health Organization describes drug-resistant infections as "one of the biggest threats to global health, food security, and development today". One reason for this is a low rate of discovery of new antibiotics. Discovery rates are low because it is difficult to make money on antibiotics, so many investors avoid this area.
"Up until the 1980s, we had a fairly vibrant antibiotics R&D space. There was lots of research going on, companies were making money from antibiotics. We had instances of drug resistance, but we had a ready pipeline of products. We’ve seen a disinvestment from that space since the 1980s and now we’re at the point where we haven’t had any new class of drugs coming to market for decades, and companies don’t see how they can make money on antibiotics. Coupled with the fact that the science is quite tricky, people are shying away from investing in it."
In order to tackle the challenge of drug-resistant infections, we need between 10 and 20 new antibiotics per decade.
David Roblin, COO of Summit Therapeutics, says that: "You will get some very learned people telling you that the industry has invented all antibiotics that there ever will be. They’re wrong."
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.

Preclinical development – first steps
The science of finding and developing new antibiotics is challenging. For antibiotics in existing classes, on average, just one drug is able to reach patients for every 15 drugs in preclinical development. The corresponding figure for brand new classes of antibiotics is 30, meaning double the failure rate.
The costs are enormous too. The expected cost for research and development on an existing class antibiotic is $1.8 billion. For a new class antibiotic, it is $2.6 billion.
"Science is not always a very linear straight line. No, we fail, we stand up, we walk again. Discovery is a chaotic process."
Governments and philanthropic organisations like Wellcome and the Gates Foundation are funding much of the early research and development of these drugs. This is often described as 'push' funding. But much, much more money is needed to see drugs through the expensive process of clinical trials, registration, and coming to market.
Unfortunately, when it comes to antibiotics, making an exciting scientific breakthrough does not translate to profit, as Anand Anandkumar, CEO of Bugworks explains: "There is no other space within the pharmaceutical industry where you don’t get rewarded for good science. This is the only field within pharmaceutical science where you come out with a drug and you don’t want it to be used too much."
The antibiotic market is broken. And without government action, there's no chance we'll #StopSuperbugs – says @wellcometrust
Clinical trials – testing new antibiotics
"Just as drug-resistant bacteria cross borders, so must the drugs that can effectively treat these diseases follow. That will mean that we all need to find a model for bringing novel drugs to market that will source these lifesaving treatments for all those in need."
Clinical trials are an essential part of new antibiotic development: this is where we see if they are safe and effective in humans. In order to get healthcare systems and hospitals to stock a new drug, manufacturers must provide evidence that the expected benefits to patients and societies from new antibiotics outweighs the massive expenditure on discovering them.
Clinical trials usually run in three phases, and not all drugs make it through to the final stage. The costs can be very high. The final phase of trials – and the trials needed after an initial product launch – account for more than 80% of total R&D spend on a new product.
When the costs of development projects that don’t make it are factored in, between $70m and $150m will be spent on Phase 1 trials for each successful launch; $150m to $200m on Phase 2; and $230m to $300m on Phase 3. Even once a product has made it through regulatory approval and into the market, $250m or more is likely to be required to ‘expand the label’. That means doing more trials to prove the product is safe and effective to use on a wider set of indications.
David Roblin, COO of Summit Therapeutics, explains why it is crucial to do the most thorough clinical testing you can, in advance of a new drug being launched.
"You can’t come with that information three or four years after launch, because it’s too late. The drug has found its position, it’s been put in reserve. You need all of this information, the new science, and the impact on healthcare costs."


Approval – registering new antibiotics
The process of registering a new antibiotic with a government drugs regulator – which needs to be done before a medicine can be legally prescribed in a particular country – can be slow, arduous and expensive. It costs, on average, $37 million.
Typically, sales of new antibiotics do not provide enough money for manufacturers to break even on all the money required to get antibiotics to and through approval. This is exacerbated by that fact that to prevent resistance quickly developing to new drugs, they need to be prescribed sparingly – which limits the amount of money that can be made.
One way of offsetting that and encouraging companies to develop and commercialise new antibiotics is through an incentive called a market entry reward. This is when manufacturers are offered rewards – usually a lump sum payment – if they successfully bring a new antibiotic to market. Governments around the world are considering this, but no one has yet taken action.
"Governments haven’t really stepped up and put the money on the table to any great extent."

The antibiotic market is broken. And without government action, there's no chance we'll #StopSuperbugs – says @wellcometrust
Marketing – reaching doctors and patients
"If you look at antibiotic product launches in the last five years, only one of those products is breaking even and making money for the manufacturer. The rest of the companies are losing money."
It can be extremely difficult to get doctors and health systems to use new antibiotics, even if they do get past regulatory hurdles. This is for a mix of reasons including a lack of professional education about new products and worries about the new drugs developing resistance.
The number of patients for which they are used is also far smaller than it would need to be for those to become profitable. This can make it even harder for investors and manufacturers to recoup their costs. Therefore, appropriate marketing is crucial. But different reports have estimated costs ranging from $40 million to $146 million for the marketing of new drugs after approval.
David Roblin, COO of Summit Therapeutics, explains: "You’ve got a prescriber base that has backed itself into the most extraordinary conservatism because of fear of resistance and because of fear of cost. It is a vicious cycle, which is forcing us to the bottom."

Treatment – saving lives
Responsible use of new antibiotics means stewardship – in other words, not overprescribing them to avoid a situation where resistance to these new drugs develops quickly. This means measures to encourage the use of a new drug are vital, but it can also make such measures harder to justify.
Jeremy Knox, Drug-Resistant Infections Policy Lead at Wellcome, explains: "Our political leaders aren’t comfortable with the optics. They don’t like the idea of this looking like a bail out of the pharmaceutical industry. They don’t like the idea of having to justify to the public why, for instance, we should be paying tens of millions of dollars for a drug which we only seem to use in very, very small quantities."
But this is an urgent issue. Antibiotic resistance threatens the most vulnerable people in society: the very young, the very elderly, those with weakened immune systems that are less able to fight infections. But it also threatens us all. Anyone undergoing surgery or chemotherapy and facing an increased risk of infection is vulnerable. And we are already seeing common infections such as gonorrhoea and urinary tract infections become increasingly difficult to treat, sometimes leading to serious complications including sepsis and even death.
"It is crucial that people stay interested, and see that antimicrobial resistance is still a problem. We haven’t won the fight. I’m working a lot with paediatricians, neonatologists. They are seriously worried – these are our most vulnerable patients."

The antibiotic market is broken. And without government action, there's no chance we'll #StopSuperbugs – says @wellcometrust
What do we need to do make sure we have new antibiotics?
Modern medicine is underpinned by antibiotics, which have saved countless lives.
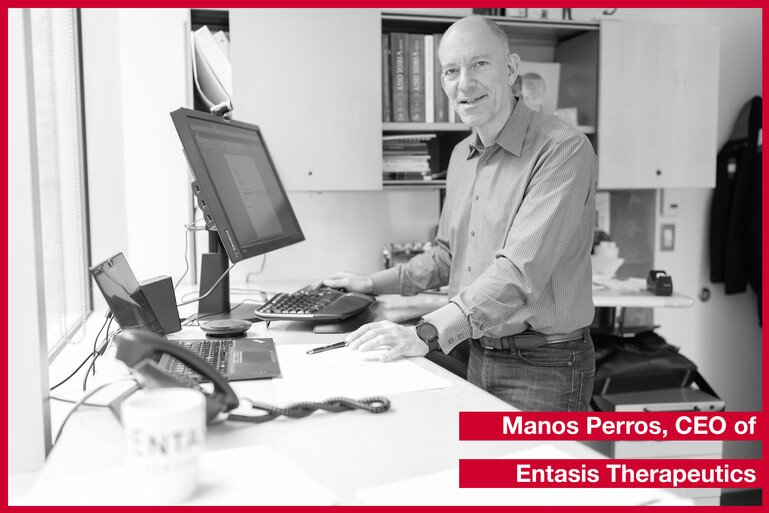
Manos Perros, CEO of Entasis Therapeutics, states that: "There is a medical need. As a society, we cannot let those patients die or suffer from drug-resistant infections when there are solutions that are accessible. We will find a way to pay for those drugs and to pay for innovators to continue investing. The question is, how quickly and exactly how?"
To solve these problems, we need concerted action. There are different options on the table. One is funding to get antibiotics to the people who need them while also making sure that investors and pharmaceutical companies don’t actually lose money.
Another suggestion is to introduce an insurance premium, with fixed annual payments for making a new antibiotic available to a health system for a period of, say, 5 or 10 years. The UK Government recently announced plans to pilot such a model in the NHS in England – although the details of this, and the amount of money it will provide, are still being worked through .
But while these options have been discussed for a number of years now, progress towards implementing them is slow. Many governments, concerned by the significant sums involved and a perception of bailing out the pharmaceutical industry, are shying away from such measures.
The precarious financial positions of many smaller companies in the field mean that the need for intervention is becoming increasingly urgent. If the idea of insurance models or lump sum payments are not attractive to governments, alternative models will be needed. New partnership models which share risk, resources and expertise across private companies, philanthropies and the private sector might also be a solution.
These are just some of the options. Whatever governments choose, they need to act now.
"If none of these [economic solutions] come through in the next one to two years, it’s game over. You’re spending hundreds of millions of dollars through CARB-X, to create a pipeline of exciting innovation in antibacterials. But if the back-end business models continue to be broken, then you have nowhere to go. It’s like building fancy cars and putting them in the parking lot and there are no gates out. What do you do with those fancy cars? They’re stuck."

This article is based on Wellcome analysis of CARB-X data and interviews with experts.
Infographics
Click on each image to enlarge it. You can download all images to use on social media or in presentations.
Click images to open gallery
Related content
- Twitter: AMR at Wellcome
